Cervical injuries
- Cervical injuries
- Radiograph sequence ABCs:
Cervical injuries
The first and most important spinal radiograph to be taken of a patient with a suspected cervical cord injury is the lateral view obtained with the x ray beam horizontal. This is much more likely than the anteroposterior view to show spinal damage and it can be taken in the emergency department without moving the supine patient. Other views are best obtained in the radiology department later. An anteroposterior radiograph and an open mouth view of the odontoid process must be taken to complete the basic series of cervical films but the latter normally requires removal of the collar and some adjustment of position, therefore the lateral x ray needs to be scrutinised first.
The lateral view should be repeated if the original radiograph does not show the whole of the cervical spine and the upper part of the first thoracic vertebra. Failure to insist on this often results in injuries of the lower cervical spine being missed. The lower cervical vertebrae are normally obscured by the shoulders unless these are depressed by traction on both arms. The traction must be stopped if it produces pain in the neck or exacerbates any neurological symptoms.
If the lower cervical spine is still not seen, a supine “swimmer’s” view should be taken. With the near shoulder depressed and the arm next to the cassette abducted, abnormalities as far down as the first or second thoracic vertebra will usually be shown. This view is not easy to interpret, and does not produce clear bony detail, but it does provide an assessment of the alignment of the cervicothoracic junction. Oblique, supine views may also help in this situation.
The interpretation of cervical spine radiographs may pose problems for the inexperienced. First, remember that the spine consists of bones (visible) and soft tissues (invisible). These are functionally arranged into three columns, anterior, middle, and posterior, which together support the stability of the spine. Next assess the radiograph using the sequence ABCs.
"A" for alignment
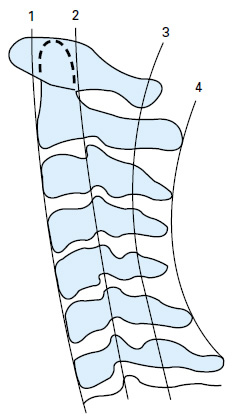
Follow four lines on the lateral radiograph:
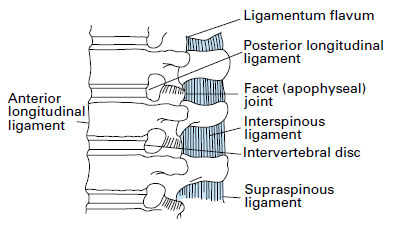
- The fronts of the vertebral bodies — anterior longitudinal ligament.
- The backs of the vertebral bodies — posterior longitudinal ligament.
- The bases of the spinous processes (ligamentum flavum) — spinolaminar line.
- The tips of the spinous processes.
The anterior arch of C1 lies in front of the odontoid process and is therefore anterior to the first line described (unless the odontoid is fractured and displaced posteriorly). Extended upwards, the spinolaminar line should cross the posterior margin of the foramen magnum. A line drawn downwards from the dorsum sellae along the surface of the clivus across the anterior margin of the foramen magnum should bisect the tip of the odontoid process.
"B" for bones
Follow the outline of each individual vertebra, and check for any steps or breaks.
"C" for cartilages
Examine the intervertebral discs and facet joints for displacement. The disc space may be widened if the annulus fibrosus is ruptured or narrowed in degenerative disc disease.
"S" for soft tissues
Check for widening of the soft tissues anterior to the spine on the lateral radiograph, denoting a prevertebral haematoma, and also widening of any bony interspaces indicating ligamentous damage — for instance separation of the spinous processes following damage to the interspinous and supraspinous ligaments posteriorly.
If the anterior or posterior displacement of one vertebra on another exceeds 3.5 mm on the lateral cervical radiograph, this must be considered abnormal. Anterior displacement of less than half the diameter of the vertebral body suggests unilateral facet dislocation; displacement greater than this indicates a bilateral facet dislocation. Atlanto-axial subluxation may be identified by an increased gap (more than 3 mm in adults and 5 mm in children) between the odontoid process and the anterior arch of the atlas on the lateral radiograph.
On the lateral radiograph, widening of the gap between adjacent spinous processes following rupture of the posterior cervical ligamentous complex denotes an unstable injury which is often associated with vertebral subluxation and a crush fracture of the vertebral body. The retropharyngeal space (at C2) should not exceed 7 mm in adults or children whereas the retrotracheal space (C6) should not be wider than 22 mm in adults or 14mm in children (the retropharyngeal space widens in a crying child).
Fractures of the anteroinferior margin of the vertebral body (“teardrop” fractures) are often associated with an unstable flexion injury and sometimes retropulsion of the vertebral body or disc material into the spinal canal. Similarly, flakes of bone may be avulsed from the anterosuperior margin of the vertebral body by the anterior longitudinal ligament in severe extension injuries.
On the anteroposterior radiograph, displacement of a spinous process from the midline may be explained by vertebral rotation secondary to unilateral facet dislocation, the spinous process being displaced towards the side of the dislocation. The spine is relatively stable in a unilateral facet dislocation, especially if maintained in extension. With a bilateral facet dislocation, the spinous processes are in line, the spine is always unstable, and the patient therefore requires extreme care when being handled. The anteroposterior cervical radiograph also provides an opportunity to examine the upper thoracic vertebrae and first to third ribs: severe trauma is required to injure these structures.
Oblique radiographs are not routinely obtained, but they do help to confirm the presence of subluxation or dislocation and indicate whether the right or left facets (apophyseal joints), or both, are affected. They may elucidate abnormalities at the cervicothoracic junction and some authorities recommend them as part of a five-view cervical spine series.
The 45˚ supine oblique view shows the intervertebral foramina and the facets but a better view for the facets is one taken with the patient log rolled 22.5˚ from the horizontal.
Flexion and extension views of the cervical spine may be taken if the patient has no neurological symptoms or signs and initial radiographs are normal but an unstable (ligamentous) injury is nevertheless suspected from the mechanism of injury, severe pain, or radiological signs of ligamentous injury. To obtain these radiographs, flexion and extension of the whole neck must be performed as far as the patient can tolerate under the supervision of an experienced doctor. Movement must cease if neurological symptoms are precipitated.
If there is any doubt about the integrity of the cervical spine on plain radiographs, CT should be performed. This provides much greater detail of the bony structures and will show the extent of encroachment on the spinal canal by vertebral displacement or bone fragments. It is particularly useful in assessing the cervicothoracic junction, the upper cervical spine and any suspected fracture or misalignment. Helical (or spiral) CT is now more available. It allows for a faster examination and also clearer reconstructed images in the sagittal and coronal planes. Many patients with major trauma will require CT of their head, chest or abdomen, and it is often appropriate to scan any suspicious or poorly seen area of their spine at the same time rather than struggle with further plain films.
MRI gives information about the spinal cord and soft tissues and will reveal the cause of cord compression, whether from bone, prolapsed discs, ligamentous damage, or intraspinal haematomas. It will also show the extent of cord damage and oedema which is of some prognostic value. Although an acute traumatic disc prolapse may be associated with bony injury, it can also occur with normal radiographs, and in these patients it is vital that an urgent MRI scan is obtained. These scans can also be used to demonstrate spinal instability, particularly in the presence of normal radiographs. MRI has superseded myelography, both in the quality of images obtained and in safety for the patient, allowing decisions to be made without the need for invasive imaging modalities. Its use may be limited by its availability and the difficulty in monitoring the acutely injured patient within the scanner.
Pathological changes in the spine — for example, ankylosing spondylitis or rheumatoid arthritis — may predispose to bony damage after relatively minor trauma and in these patients further radiological investigation and imaging must be thorough.
See also
- At the accident:
- History and epidemiology of spinal cord injury
- Spinal injuries management at the scene of the accident
- Evacuation and initial management at hospital:
- Evacuation and transfer to hospital of patients with spinal cord injuries
- Initial management of patients with spinal cord injuries at the receiving hospital
- Neurological assessment of patients with spinal cord injuries
- Spinal shock after severe spinal cord injury
- Partial spinal cord injury syndromes
- Radiological investigations:
- Initial radiography of patients with spinal cord injuries
- Cervical injuries
- Thoracic and lumbar injuries
- Early management and complications of spinal cord injuries — I:
- Respiratory complications
- Cardiovascular complications
- Prophylaxis against thromboembolism
- Initial bladder management
- The gastrointestinal tract
- Use of steroids and antibiotics
- The skin and pressure areas
- Care of the joints and limbs
- Later analgesia
- Trauma re-evaluation
- Early management and complications of spinal cord injuries — II:
- The anatomy of spinal cord injury
- The spinal injury (cervical, thoracic and lumbar spine)
- Transfer to a spinal injuries unit
- Medical management in the spinal injuries unit:
- The cervical spine injuries
- The cervicothoracic junction injuries
- Thoracic injuries
- Thoracolumbar and lumbar injuries
- Deep vein thrombosis and pulmonary embolism
- Autonomic dysreflexia
- Biochemical disturbances
- Para-articular heterotopic ossification
- Spasticity
- Contractures
- Pressure sores
- Urological management of patients with spinal cord injury:
- Nursing for people with spinal cord lesion:
- Physiotherapy after spinal cord injury:
- Respiratory management
- Mobilisation into a wheelchair
- Rehabilitation
- Recreation
- Incomplete lesions
- Children
- Occupational therapy after spinal cord injury:
- Hand and upper limb management
- Home resettlement
- Activities of daily living
- Communication
- Mobility
- Leisure
- Work
- Social needs of patient and family:
- Transfer of care from hospital to community:
- Education of patients
- Teaching the family and community staff
- Preparation for discharge from hospital
- Easing transfer from hospital to community
- Travel and holidays
- Follow-up
- Later management and complications after spinal cord injury — I:
- Late spinal instability and spinal deformity
- Pathological fractures
- Post-traumatic syringomyelia (syrinx, cystic myelopathy)
- Pain
- Sexual function
- Later management and complications after spinal cord injury — II:
- Later respiratory management of high tetraplegia
- Psychological factors
- The hand in tetraplegia
- Functional electrical stimulation
- Ageing with spinal cord injury
- Prognosis
- Spinal cord injury in the developing world: