Partial spinal cord injury syndromes
Partial spinal cord injury syndromes
Neurological symptoms and signs may not fit a classic pattern or demonstrate a clear neurological level. For this reason, some cord injuries are not infrequently misdiagnosed and attributed to hysterical or conversion paralysis. Neurological symptoms or signs must not be dismissed until spinal cord injury has been excluded by means of a thorough examination and appropriate clinical investigations.
Assessment of the level and completeness of the spinal cord injury allows a prognosis to be made. If the lesion is complete from the outset, recovery is far less likely than in an incomplete lesion.
Following trauma to the spinal cord and cauda equina there are recognised patterns of injury, and variations of these may present in the emergency department.
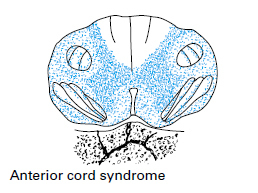
Anterior cord syndrome
The anterior part of the spinal cord is usually injured by a flexion-rotation force to the spine producing an anterior dislocation or by a compression fracture of the vertebral body with bony encroachment on the vertebral canal. There is often anterior spinal artery compression so that the corticospinal and spinothalamic tracts are damaged by a combination of direct trauma and ischaemia. This results in loss of power as well as reduced pain and temperature sensation below the lesion.
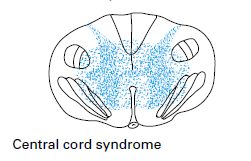
Central cord syndrome
This is typically seen in older patients with cervical spondylosis. A hyperextension injury, often from relatively minor trauma, compresses the spinal cord between the irregular osteophytic vertebral body and the intervertebral disc anteriorly and the thickened ligamentum flavum posteriorly. The more centrally situated cervical tracts supplying the arms suffer the brunt of the injury so that classically there is a flaccid (lower motor neurone) weakness of the arms and relatively strong but spastic (upper motor neurone) leg function. Sacral sensation and bladder and bowel function are often partially spared.
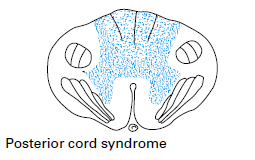
Posterior cord syndrome
This syndrome is most commonly seen in hyperextension injuries with fractures of the posterior elements of the vertebrae. There is contusion of the posterior columns so the patient may have good power and pain and temperature sensation but there is sometimes profound ataxia due to the loss of proprioception, which can make walking very difficult.
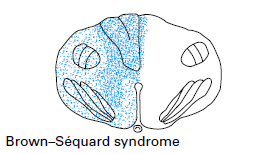
Brown–Séquard syndrome
Classically resulting from stab injuries but also common in lateral mass fractures of the vertebrae, the signs of the Brown-Séquard syndrome are those of a hemisection of the spinal cord. Power is reduced or absent but pain and temperature sensation are relatively normal on the side of the injury because the spinothalamic tract crosses over to the opposite side of the cord. The uninjured side therefore has good power but reduced or absent sensation to pin prick and temperature.
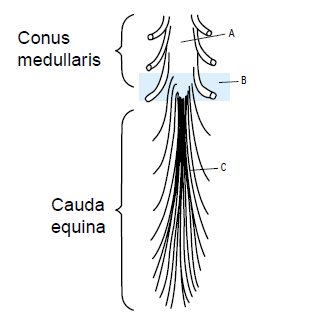
Conus medullaris syndrome
The effect of injury to the sacral cord (conus medullaris) and lumbar nerve roots is usually loss of bladder, bowel and lower limb reflexes. Lesions high in the conus may occasionally represent upper motor neurone defects and function may then be preserved in the sacral reflexes, for example the bulbocavernosus and micturition reflexes.
Cauda equina syndrome
Injury to the lumbosacral nerve roots results in areflexia of the bladder, bowel, and lower limbs.
The final phase in the diagnosis of spinal trauma entails radiology of the spine to assess the level and nature of the injury.
See also
- At the accident:
- History and epidemiology of spinal cord injury
- Spinal injuries management at the scene of the accident
- Evacuation and initial management at hospital:
- Evacuation and transfer to hospital of patients with spinal cord injuries
- Initial management of patients with spinal cord injuries at the receiving hospital
- Neurological assessment of patients with spinal cord injuries
- Spinal shock after severe spinal cord injury
- Partial spinal cord injury syndromes
- Radiological investigations:
- Initial radiography of patients with spinal cord injuries
- Cervical injuries
- Thoracic and lumbar injuries
- Early management and complications of spinal cord injuries — I:
- Respiratory complications
- Cardiovascular complications
- Prophylaxis against thromboembolism
- Initial bladder management
- The gastrointestinal tract
- Use of steroids and antibiotics
- The skin and pressure areas
- Care of the joints and limbs
- Later analgesia
- Trauma re-evaluation
- Early management and complications of spinal cord injuries — II:
- The anatomy of spinal cord injury
- The spinal injury (cervical, thoracic and lumbar spine)
- Transfer to a spinal injuries unit
- Medical management in the spinal injuries unit:
- The cervical spine injuries
- The cervicothoracic junction injuries
- Thoracic injuries
- Thoracolumbar and lumbar injuries
- Deep vein thrombosis and pulmonary embolism
- Autonomic dysreflexia
- Biochemical disturbances
- Para-articular heterotopic ossification
- Spasticity
- Contractures
- Pressure sores
- Urological management of patients with spinal cord injury:
- Nursing for people with spinal cord lesion:
- Physiotherapy after spinal cord injury:
- Respiratory management
- Mobilisation into a wheelchair
- Rehabilitation
- Recreation
- Incomplete lesions
- Children
- Occupational therapy after spinal cord injury:
- Hand and upper limb management
- Home resettlement
- Activities of daily living
- Communication
- Mobility
- Leisure
- Work
- Social needs of patient and family:
- Transfer of care from hospital to community:
- Education of patients
- Teaching the family and community staff
- Preparation for discharge from hospital
- Easing transfer from hospital to community
- Travel and holidays
- Follow-up
- Later management and complications after spinal cord injury — I:
- Late spinal instability and spinal deformity
- Pathological fractures
- Post-traumatic syringomyelia (syrinx, cystic myelopathy)
- Pain
- Sexual function
- Later management and complications after spinal cord injury — II:
- Later respiratory management of high tetraplegia
- Psychological factors
- The hand in tetraplegia
- Functional electrical stimulation
- Ageing with spinal cord injury
- Prognosis
- Spinal cord injury in the developing world: