Early management and complications of spinal cord injuries — I
Respiratory complications
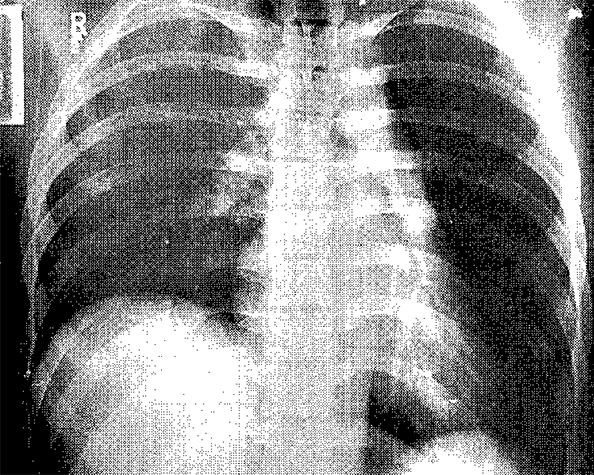
Respiratory insufficiency is common in patients with injuries of the cervical cord. If the neurological lesion is complete the patient will have paralysed intercostal muscles and will have to rely on diaphragmatic respiration. Partial paralysis of the diaphragm may also be present, either from the outset or after 24–48 hours if ascending post-traumatic cord oedema develops. In patients with injuries of the thoracic spine, respiratory impairment often results from associated rib fractures, haemopneumothorax, or pulmonary contusion; there may also be a varying degree of intercostal paralysis depending on the neurological level of the lesion.
Sputum retention occurs readily during the first few days after injury, particularly in patients with high lesions and in those with associated chest injury. The inability to produce an effective cough impairs the clearing of secretions and commonly leads to atelectasis. The loss of lung compliance contributes to difficulty in breathing and leads to a rapid exhaustion of the inspiratory muscles. Abnormal distribution of gases and blood (ventilation-perfusion mismatch) also occurs in the lungs of tetraplegic patients, producing further respiratory impairment.
Patients normally need to be nursed in the recumbent position because of the spinal injury, and even if spinal stabilisation has been undertaken, tetraplegics and high paraplegics should still not be sat up, as this position limits the excursion of the diaphragm and reduces their vital capacity.
Causes of respiratory insufficiency:
| In tetraplegia | In paraplegia |
| - Intercostal paralysis - Partial phrenic nerve palsy (immediate, delayed) - Impaired ability to expectorate - Ventilation-perfusion mismatch |
- Variable intercostal paralysis according to level of injury - Associated chest injuries (rib fractures, pulmonary contusion, haemopneumothorax) |
Regular chest physiotherapy with assisted coughing and breathing exercises is vital to prevent atelectasis and pulmonary infection. Respiratory function should be monitored by measuring the oxygen saturation, vital capacity, and arterial blood gases. A vital capacity of less than 15 ml/kg body weight with a rising Pco2 denotes respiratory failure, and should alert clinicians to support respiration (non-invasive pressure support may suffice). Bi-level support is preferable to continuous positive airway pressure (CPAP) and may avoid resorting to full ventilation. This mode of respiratory support may also assist in weaning the patient from full ventilation. The inspired air must be humified, as in full ventilation, otherwise secretions will become viscid and difficult to clear.
If atelectasis necessitates bronchoscopy this is a safe procedure which can be performed without undue movement of the patient’s neck by using modern fibreoptic instruments. If the patient is already intubated the fibreoptic bronchoscope can be passed down the tracheal tube. Although early tracheostomy is best avoided in the first instance, as ventilation is sometimes needed for a few days only, it should not be delayed unnecessarily. It allows easy access for airways toilet and facilitates weaning from the ventilator. Minitracheostomy can be useful if the problem is purely one of retained secretions.
Nurse in recumbent position to:
- Protect the spinal cord
- Maximise diaphragmatic excursion
A patient whose respiratory function is initially satisfactory after injury but then deteriorates should regain satisfactory ventilatory capacity once spinal cord oedema subsides. Artificial ventilation should therefore not be withheld, except perhaps in the elderly and infirm where treatment is likely to be prolonged and unsuccessful. By involving the patients and their relatives, artificial ventilation may sometimes be withheld in this situation and the patient kept comfortable. If there is a risk of deterioration in respiratory function during transit, an anaesthetist must accompany the patient. Cardiac failure after spinal cord injury is often secondary to respiratory failure.
Physiotherapy:
- Regular chest physiotherapy
- Assisted coughing
Weaning from pressure support or full ventilation should be managed with the patient in the recumbent position to take advantage of maximal diaphragmatic excursion.
Improved cardiopulmonary resuscitation:
- Increased number of high lesion tetraplegics now survive the acute injury
- Many require long-term ventilatory support
With increasing public awareness of cardiopulmonary resuscitation and the routine attendance of paramedics at accidents, patients with high cervical injuries and complete phrenic nerve paralysis are surviving. These patients often require long-term ventilatory support, and this can be achieved either mechanically or electronically by phrenic nerve pacing in selected cases, although not all high tetraplegics are suitable for phrenic nerve pacing. If the spinal cord injury causes damage to the anterior horn cells of C3, C4 and C5, the phrenic nerve will have lower motor neurone damage and be incapable of being stimulated. The necessity for long-term ventilation should be no bar to the patient returning home, and patients are now surviving on domiciliary ventilation with a satisfactory quality of life (see Chapter 14).
Cardiovascular complications
Haemorrhage from associated injuries is the commonest cause of post-traumatic shock and must be treated vigorously. However, it must be realised that in traumatic tetraplegia the thoracolumbar (T1–L2) sympathetic outflow is interrupted. Vagal tone is therefore unopposed and the patient can become hypotensive and bradycardic. Even in paraplegia, sympathetic paralysis below the lesion can produce hypotension, referred to as neurogenic shock. If shock is purely neurogenic in origin, patients can mistakenly be given large volumes of intravenous fluid and then develop pulmonary oedema.
Pharyngeal suction and tracheal intubation stimulate the vagus, and in high cord injuries can produce bradycardia, which may result in cardiac arrest. To prevent this it is wise to give atropine or glycopyrronium in addition to oxygen before suction and intubation are undertaken and also whenever the heart rate falls below 50 beats/minute. Clinicians, however, must be aware of the possible toxic effects when the standard dose of 0.6 mg atropine is used repeatedly. If the systolic blood pressure cannot maintain adequate perfusion pressure to produce an acceptable flow of urine after any hypovolaemia has been corrected, then inotropic medication with dopamine should be started.
![]() Attention! Beware of overinfusion in patients with neurogenic shock.
Attention! Beware of overinfusion in patients with neurogenic shock.
Treat:
- Bradycardia <50 beats/min
- Hypotension <80 mm Hg systolic or adequate urinary excretion not maintained
Cardiac arrest due to sudden hyperkalaemia after the use of a depolarising agent such as suxamethonium for tracheal intubation is a risk in patients with spinal cord trauma between three days and nine months after injury. If muscle relaxation is required for intubation during this period a non-depolarising muscle relaxant such as rocuronium is indicated to avoid the risk of hyperkalaemic cardiac arrest.
![]() Attention! Risk of hyperkalaemic cardiac arrest. Beware — do not give suxamethonium from three days to nine months following spinal cord injury as grave risk of hyperkalaemic cardiac arrest.
Attention! Risk of hyperkalaemic cardiac arrest. Beware — do not give suxamethonium from three days to nine months following spinal cord injury as grave risk of hyperkalaemic cardiac arrest.
Prophylaxis against thromboembolism
Newly injured tetraplegic or paraplegic patients have a very high risk of developing thromboembolic complications. The incidence of pulmonary embolism reaches a maximum in the third week after injury and it is the commonest cause of death in patients who survive the period immediately after the injury.
Anticoagulation:
- Apply antiembolism stockings
- If there are no medical or surgical contraindications give low molecular weight heparin within 72 hours
If there are no other injuries or medical contraindications, such as head or chest injury, antiembolism stockings should be applied to all patients and anticoagulation started within the first 72 hours of the accident. Low molecular weight heparin for 8–12 weeks is usually preferred to warfarin.
Initial bladder management
After a severe spinal cord injury the bladder is initially acontractile, and untreated the patient will develop acute retention. The volume of urine in the bladder should never be allowed to exceed 500 ml because overstretching the detrusor muscle can delay the return of bladder function. If the patient is transferred to a spinal injuries unit within a few hours after injury it may be possible to defer catheterisation until then, but if the patient drank a large volume of fluid before injury this is unwise. In these circumstances, and in patients with multiple injuries, the safest course is to pass a small bore (12–14 Ch) 10 ml balloon silicone Foley catheter.
Initial bladder management:
- Avoid overdistension
- 12–14 Ch silicone Foley catheter
The gastrointestinal tract
The patient should receive intravenous fluids for at least the first 48 hours, as paralytic ileus usually accompanies a severe spinal injury. A nasogastric tube is passed and oral fluids are forbidden until normal bowel sounds return. If paralytic ileus becomes prolonged the abdominal distension splints the diaphragm and, particularly in tetraplegic patients, this may precipitate a respiratory crisis if not relieved by nasogastric aspiration. If a tetraplegic patient vomits, gastric contents are easily aspirated because the patient cannot cough effectively. Ileus may also be precipitated by an excessive lumbar lordosis if too bulky a lumbar pillow is used for thoracolumbar injuries.
Acute peptic ulceration, with haemorrhage or perforation, is an uncommon but dangerous complication after spinal cord injury, and for this reason proton pump inhibitors or H2-receptor antagonists should be started as soon as possible after injury and continued for at least three weeks. When perforation occurs it often presents a week after injury with referred pain to the shoulder, but during the stage of spinal shock guarding and rigidity will be absent and tachycardia may not develop. A supine decubitus abdominal film usually shows free gas in the peritoneal cavity.
![]() Attention! Beware of paralytic ileus: patients should receive intravenous fluids for at least the first 48 hours after injury.
Attention! Beware of paralytic ileus: patients should receive intravenous fluids for at least the first 48 hours after injury.
Risk of acute peptic ulceration with haemorrhage or perforation:
- Treat with proton pump inhibitor or H2-receptor antagonist
- Continue treatment for three weeks
Use of steroids and antibiotics
An American study (NASCIS 2) suggested that a short course of high-dose methylprednisolone started within the first eight hours after closed spinal cord injury improves neurological outcome. A later study (NASCIS 3) suggested that patients commencing methylprednisolone within 3 hours of injury should have a 24-hour treatment regimen, but for patients commencing treatment 3–8 hours after injury the treatment period should be extended to 48 hours. Recently the use of steroids has been challenged, and their use has not been universally accepted. Policy concerning steroid treatment should be agreed with the local spinal injuries unit.
Antibiotics are not normally indicated for the prevention of either urinary or pulmonary infection. Only established infections should be treated.
Drug treatment in spinal cord injury:
- Consult your spinal unit for advice
- If methylprednisolone is given, administer at the earliest opportunity: 30 mg/kg intravenously and then infusion of 5.4 mg/kg/h for 23 hours if commenced within 3 hours of injury. If treatment is started 3–8 hours after injury, the infusion is continued for 47 hours.
The skin and pressure areas
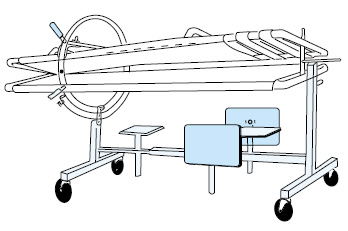
When the patient is transferred from trolley to bed the whole of the back must be inspected for bruising, abrasions, or signs of pressure on the skin. The patient should be turned every two hours between supine and right and left lateral positions to prevent pressure sores, and the skin should be inspected at each turn. Manual turning can be achieved on a standard hospital bed, by lifting patients to one side (using the method described in chapter 8 on nursing) and then log rolling them into the lateral position. Alternatively, an electrically driven turning and tilting bed can be used. Another convenient solution is the Stryker frame, in which a patient is “sandwiched” between anterior and posterior sections, which can then be turned between the supine and prone positions by the inbuilt circular turning mechanism, but tetraplegic patients may not tolerate the prone position.
Nursing care requires the use of pillows to separate the legs, maintain alignment of the spine, and prevent the formation of contractures. In injuries of the cervical spine a neck roll is used to maintain cervical lordosis. A lumbar pillow maintains lumbar lordosis in thoracolumbar injuries.
Care of the joints and limbs
The joints must be passively moved through the full range each day to prevent stiffness and contractures in those joints which may later recover function and to prevent contractures elsewhere, which might interfere with rehabilitation. Splints to keep the tetraplegic hand in the position of function are particularly important. Foot drop and equinus contracture are prevented by placing a vertical pillow between the foot of the bed and the soles of the feet.
Skeletal traction of lower limb fractures should be avoided, but early internal or external fixation of limb fractures is often indicated to assist nursing, particularly as pressure sores in anaesthetic areas may develop unnoticed in plaster casts.
Joint and limb care:
- Daily passive movement of joints
- Splints for hands of tetraplegic patients
- Early internal fixation of limb fractures often required
Later analgesia
In the ward environment, diamorphine administered as a low-dose subcutaneous constant infusion, once the correct initial dose has been titrated, gives excellent pain relief, especially if combined with a non-steroidal anti-inflammatory drug. Close observation is essential and naloxone must always be available in case of respiratory depression.
It diamorphine is unavailable, a syringe-driven intraveneous morphine infusion can be used.
Trauma re-evaluation
Trauma patients may be obtunded by head injury or distracted by major fractures and wounds. As a result, some injuries associated with high morbidity, for example scaphoid fracture, may not generate symptoms during early management. The diagnosis of such injuries can be difficult in any trauma patient but in spinal cord injury, the symptoms and signs are often abolished by sensory and motor impairments. Furthermore, some of these injuries compromise rehabilitation and the ultimate functional outcome. Daily re-evaluation of trauma patients helps to overcome these diagnostic difficulties and is very important during the first month after injury.
Trauma re-evaluation:
- Following spinal cord trauma, occult injuries can easily compromise recovery or aggravate disability. Complete clinical re-assessments must be performed regularly during the first month after injury.
See also
- At the accident:
- History and epidemiology of spinal cord injury
- Spinal injuries management at the scene of the accident
- Evacuation and initial management at hospital:
- Evacuation and transfer to hospital of patients with spinal cord injuries
- Initial management of patients with spinal cord injuries at the receiving hospital
- Neurological assessment of patients with spinal cord injuries
- Spinal shock after severe spinal cord injury
- Partial spinal cord injury syndromes
- Radiological investigations:
- Initial radiography of patients with spinal cord injuries
- Cervical injuries
- Thoracic and lumbar injuries
- Early management and complications of spinal cord injuries — I:
- Respiratory complications
- Cardiovascular complications
- Prophylaxis against thromboembolism
- Initial bladder management
- The gastrointestinal tract
- Use of steroids and antibiotics
- The skin and pressure areas
- Care of the joints and limbs
- Later analgesia
- Trauma re-evaluation
- Early management and complications of spinal cord injuries — II:
- The anatomy of spinal cord injury
- The spinal injury (cervical, thoracic and lumbar spine)
- Transfer to a spinal injuries unit
- Medical management in the spinal injuries unit:
- The cervical spine injuries
- The cervicothoracic junction injuries
- Thoracic injuries
- Thoracolumbar and lumbar injuries
- Deep vein thrombosis and pulmonary embolism
- Autonomic dysreflexia
- Biochemical disturbances
- Para-articular heterotopic ossification
- Spasticity
- Contractures
- Pressure sores
- Urological management of patients with spinal cord injury:
- Nursing for people with spinal cord lesion:
- Physiotherapy after spinal cord injury:
- Respiratory management
- Mobilisation into a wheelchair
- Rehabilitation
- Recreation
- Incomplete lesions
- Children
- Occupational therapy after spinal cord injury:
- Hand and upper limb management
- Home resettlement
- Activities of daily living
- Communication
- Mobility
- Leisure
- Work
- Social needs of patient and family:
- Transfer of care from hospital to community:
- Education of patients
- Teaching the family and community staff
- Preparation for discharge from hospital
- Easing transfer from hospital to community
- Travel and holidays
- Follow-up
- Later management and complications after spinal cord injury — I:
- Late spinal instability and spinal deformity
- Pathological fractures
- Post-traumatic syringomyelia (syrinx, cystic myelopathy)
- Pain
- Sexual function
- Later management and complications after spinal cord injury — II:
- Later respiratory management of high tetraplegia
- Psychological factors
- The hand in tetraplegia
- Functional electrical stimulation
- Ageing with spinal cord injury
- Prognosis
- Spinal cord injury in the developing world: