Later management and complications after spinal cord injury — II
Later respiratory management of high tetraplegia
As a result of improved first aid at the scenes of accidents an increasing number of patients are surviving with neurological lesions above C4, who have therefore lost diaphragmatic function and can no longer breathe. These patients require long-term ventilatory support. Modern portable ventilators that use a 12-volt battery can be mounted on a wheelchair, allowing the patient a degree of freedom and independence. Speech is possible with an uncuffed tracheostomy tube around which air can escape to the larynx.
In a small number of these patients the anterior horn cells of the phrenic nerve are spared and it may be possible to implant a phrenic nerve stimulator to achieve ventilation. The advantages of electrophrenic respiration are that it is more physiological than positive pressure ventilation and it gives the patient more freedom, the equipment being much lighter than a mechanical ventilator. The disadvantages are that stimulation often cannot be sustained for 24 hours, a rest period overnight is necessary on a mechanical ventilator, and the implant is expensive. The long-term ventilator-dependent patient needs 24-hour care by a team of carers competent to undertake endotracheal suction, but not necessarily including a qualified nurse.
High tetraplegia:
- Improved first aid has increased number of high tetraplegics surviving scene of accident
- If lesion above C4, diaphragmatic function lost
Chronic ventilation:
- Electrophrenic respiration (diaphragmatic pacing)
- Mechanical "domiciliary" ventilation
| Advantages of electrophrenic respiration | Drawbacks of electrophrenic respiration |
| - More physiological than positive pressure ventilation - More portable than positive pressure ventilation |
- Often stimulation cannot be sustained, necessitating rest period overnight on mechanical ventilator - More expensive |
Psychological factors
In the acute stage of spinal cord injury an individual may experience a range of emotions such as numbness, despair, fear, hope, and anger. This emotional turmoil is often chaotic and disorganised. It may be further complicated by the enforced period of bed rest during which a state of sensory deprivation ensues. Following this early period anxiety and depression may become apparent in approximately one third of individuals. The frustrations associated with the physical limitations of such a severe injury are compounded by the fact that most patients are young and before injury led active lives, often expressing themselves mainly through physical activities. The sudden inability to continue in this manner and the need to lead a more ordered life can mean a very difficult and prolonged period of adjustment. Failure to recognise that this process can continue for as long as two or three years may damage the process of rehabilitation and the patient’s ultimate resettlement. The patient needs time to come to terms with his or her new status and to make decisions about the future without undue pressure.
Psychological factors:
| Acute stage | Later stages |
| - Initial stress reaction - Sensory deprivation |
- Anxiety and depression - Post-traumatic stress disorder - Cognitive problems - Detecting psychological problems - Appropriate referral - Family - Psychological support and therapy |
Detection of these psychological problems is vital in order to make appropriate referral. Psychological support and therapy has been shown to be very effective in improving mood and also later adjustment in individuals with spinal cord injury. Other psychological problems that may be present following injury include post-traumatic stress disorder in which an individual continually relives their accident and marked problems with memory, concentration, and problem solving.
Detection of these problems and the provision of psychological therapy will enable an individual to overcome them, as well as improving the process of rehabilitation. The family of the patient may also experience psychological difficulties and as a result benefit from support and intervention. A holistic approach including a psychological perspective will not only benefit the patient and their family but will improve rehabilitation and ultimately the long-term emotional outcome of those individuals who sustain this type of injury.
Good psychological support improves:
- Adjustment to injury
- Process of rehabilitation
- Long-term outcome
The hand in tetraplegia
Most tetraplegic patients give priority to restoring hand function. Much can be done to improve function in these patients with tendon transfer surgery and functional electrical stimulation. Patients should be at least 12 months post-injury and have been neurologically stable for 6 months prior to surgical intervention. They should be in good general health and marked spasticity is a relative contraindication to surgery. Fixed hand contractures are also a contraindication as they will compromise the quality of result. Soft, mobile hands with a full passive range of motion in the joints are ideal.
Aims to restore:
- Active elbow extension
- Wrist extension
- Hand opening
- Hand grasp:
- Palmar grasp
- Lateral pinch
- Improved ability to perform acts of daily living
The presence of sensation is important for the functional result and determines whether bi-manual tasks can be done easily. In the absence of sensation, vision replaces sensation: the patient can only concentrate on one hand at a time.
Two-thirds of tetraplegic patients are unable to extend their elbows. Restoration of elbow extension enables the patient to reach overhead and also facilitates wheelchair skills, for pressure relief and transfers. The posterior third of the deltoid muscle is usually used and its tendon is connected to the triceps tendon at the elbow. The result depends on the initial strength of the deltoid muscle.
Wrist extension is a vital prerequisite to hand (palmar) grasp and lateral pinch (key grip).
In C5 or high C6 patients, lateral pinch or key grip, as described by Moberg, is possible during wrist extension by tenodesing the flexor pollicis longus to the lower end of the radius and stabilising the interphalangeal joint. Wrist extension is achieved by transferring brachioradialis into carpi extensor radialis brevis. With the wrist extended the thumb will oppose the radial side of the index finger.
In lower C6 lesions or better, functional hand grasp may be restored with a passive flexor tenodesis. Active wrist extension is achieved, by transferring the brachioradialis into the insertion of extensor carpi radialis brevis. If wrist extension is active and the extensor carpi radialis longus and brevis are normally innervated, extensor carpi radialis longus may be transferred into the flexor digitorum profundus to achieve finger flexion. Brachioradialis may be transferred into flexor pollicis longus for thumb flexion.
Further surgical procedures include implantation of the NeuroControl Freehand system (see below), which is an upper limb neuroprosthesis suitable for C5 and upper C6 spinal cord injured patients, and procedures to achieve an intrinsic balance and improve hand function in lower cervical injuries.
Factors in selection for surgery:
| Absolute prerequisites | Relative factors in selection |
| - Neurological level C5 and below - No change in muscle power for at least 6 months - Well motivated patient |
- Adequate sensation in hand - Minimal or no spasticity - Minimal or no contractures |
Functional electrical stimulation
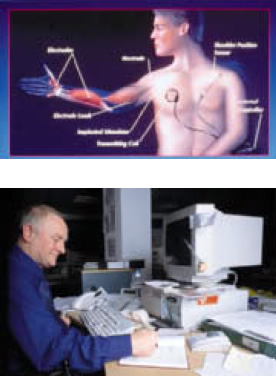
Following spinal cord injury, lower motor neurone pathways may remain intact and have the potential to be electrically stimulated. Functional electrical stimulation (FES) of paralysed muscles to restore function is becoming more commonly used, although only a few systems are commercially available, such as the NeuroControl Freehand system, the Handmaster, and the ODFS. The NeuroControl Freehand system consists of an implantable receiver placed subcutaneously on the pectoralis major fascia. Eight electrodes are attached to specific muscles to achieve hand opening, lateral pinch, and hand grasp. The implant is controlled by moving the opposite shoulder, which is connected by a lever to a "joystick" located on the central chest. These movements generate signals, which are analysed by a control unit which then provides output signals to the externally placed radiofrequency coil, thereby initiating hand opening and closing and grasp patterns. Functional grasp patterns improve the user ability to perform specific activities of daily living.
Functional electrical stimulation. Attempts to replace or improve missing functions, using the body’s own muscles, through:
- External devices
- Implanted systems
The Handmaster is a splint-based FES device for C5 tetraplegics. The forearm and wrist are held in a neutral position by the splint, on the inner surface of which are saline-soaked electrodes. These are placed over finger and thumb extensors and a thumb abductor, using pre-set patterns of stimulation to open and close the hand. The system is designed for holding objects such as a fork or pen.
The Odstock Dropped Foot Stimulator (ODFS) is a single channel stimulator designed to correct dropped foot following incomplete spinal cord injury. Self-adhesive electrodes are placed over the common peroneal nerve as it passes over the head of the fibula. Stimulation is timed to the gait cycle using a pressure switch placed in the shoe. Trials of the ODFS have shown that walking can be less effort, faster, and safer.
The benefits of FES include an increase in muscle bulk and blood flow in the legs. This may be at the expense of spasms becoming stronger as muscular strength increases, but the majority of people find that their spasms are more predictable and less frequent, especially in the period immediately after FES.
Re-training muscles calls for a long-term commitment, and places great demands on the patient’s time. Ambulation remains a distant goal for people with complete injuries, although cycling on recumbent tricycles is feasible. Systems in incomplete injuries can significantly improve walking speed and performance.
The practical uses of electrical stimulation to achieve function (FES):
| Patient group | Stimulated function | Stimulator type | Control mechanism |
| Neurologically incomplete | Control of foot drop +\- knee extension, hip extension | ODFS (Odstock Dropped Foot Stimulator), with 1 or 2 channel external electrodes | Controlled by foot switch |
| Respiration (there are three systems commercially available) | Implanted electrodes onto phrenic nerves | Preprogrammed | |
| Neurologically complete | Bladder (bowel and erection) | NeuroControl Vocare bladder system (sacral anterior root stimulator — SARS) — implanted electrodes onto 2nd, 3rd and 4th anterior sacral nerve roots | Preprogrammed (3 options) |
| Ejaculation | Implanted electrodes onto hypogastric plexus on sacrum | Preprogrammed | |
| Hand function (palmar and lateral grip, grasp and release) | Handmaster external system with surface electrodes | Preprogrammed triggered by pressing button | |
| NeuroControl Freehand implanted system with 8 electrodes on muscles of forearm and hand | Joystick attached to contralateral shoulder | ||
| Research | |||
| Lower limbs (used for lower limb exercise, blood flow, skin quality, bone density and research into ambulation) | Surface electrodes | External feedback control system | |
| Implanted anterior lumbar and sacral nerve roots | External multi-option preprogrammed controller | ||
| Normal or Abnormal | Implanted electrodes on muscle surface | External controller | |
Ageing with spinal cord injury
The spinal cord injury population is ageing, partly because survival rates following injury have improved, and partly because the percentage of older people sustaining spinal cord injury has increased. The ageing spinal cord injured patient may present with several problems. In the case of people injured at a young age, if their parents are the carers, they will eventually be unable to cope, and may need care themselves.
The majority of patients will put increased strain on their upper limbs due to propelling their wheelchair, transferring or walking with crutches and orthoses, and often after 15–20 years will have increasing pain and discomfort in the joints of the upper limb, particularly the shoulders. They may then become less independent and have to consider using additional aids such as transfer boards, hoists, and mechanical aids to lift their chairs into their car. They may have to change from a manual to a motorised wheelchair, and have a vehicle which they can drive from their wheelchair. A change in lifestyle to reduce the number of transfers, further domestic modifications, and an increased level of care may be necessary. For those in employment, a reduction in the number of hours worked or the taking of early retirement may be inevitable. A person who has previously coped well with a severe disability for most of their life may begin to have very significant problems because of the effect of ageing.
Prognosis
It is important to indicate the probable degree of recovery at an early stage to both patient and relatives to make planning for the future realistic. The question of financial compensation will often arise in accident cases, and an informed opinion will be required on the degree of functional recovery that is likely and the effect on life expectancy. Recovery after a complete cord lesion is far less likely than after an incomplete lesion, but it is unwise to predict non-recovery too early, as some patients with an incomplete injury may initially appear to be totally paralysed because of spinal cord oedema and contusion, which later resolves. Forecasting the outcome in patients with an incomplete lesion is notoriously difficult. Too optimistic a prognosis may lead to great disappointment, with loss of morale and decreased interest in rehabilitation when hopes are unfulfilled. Contrary to a widely held view, however, neurological improvement can very occasionally be seen later than two years after injury, not only with nerve root and cauda equina lesions but also with cord injuries.
Mortality in acutely injured patients managed in a spinal injuries unit is now less than 5%. Death within the first few days is likely to be from respiratory failure, particularly in high tetraplegia. The presence of multiple injuries, age, and previous health of the patient all play a part. In patients surviving the period immediately after injury pulmonary embolism is still the commonest cause of death in the acute phase.
With the modern management of spinal cord injury, particularly improvements in the management of the urinary tract and pressure sore prevention, life expectancy has improved over recent years; as a consequence pathologies experienced by the general population such as atherosclerosis and its complications, and malignancy, are now major causes of late death, as well as respiratory causes, particularly in tetraplegic patients.
Neurological recovery:
- Much less likely after complete lesion
- In incomplete lesions recovery may occur for two years or more
Great progress has been made in the care of patients with spinal cord injuries since the 1940s, when spinal injuries units were first established. There has been a remarkable decrease in complications by using the multidisciplinary approach provided by such units, yet some patients are still denied referral. Unless complete recovery occurs, patients should have lifelong hospital outpatient follow up but with emphasis on continuing care and support in the community.
Life expectancy in years for people with spinal cord injuries who survive at least one year after injury, according to current age and neurological category (Frankel grades — see box below):
| Current age (years) | Normal* | C1–C4 (Frankel grade A, B, C) | C5–C8 (Frankel grade A, B, C) | T1–S5 (Frankel grade A, B, C) | (Frankel grade D) |
| 5 | 70.8 | 45.0 | 52.0 | 59.5 | 36.0 |
| 10 | 65.9 | 40.5 | 47.3 | 53.7 | 58.2 |
| 15 | 61.0 | 36.1 | 42.6 | 49.0 | 53.4 |
| 20 | 56.3 | 32.8 | 38.6 | 44.8 | 49.0 |
| 25 | 51.6 | 29.9 | 34.7 | 40.8 | 44.7 |
| 30 | 46.9 | 26.8 | 30.7 | 36.7 | 40.5 |
| 35 | 42.2 | 23.7 | 27.0 | 32.7 | 36.1 |
| 40 | 37.6 | 20.9 | 23.6 | 28.8 | 31.7 |
| 45 | 33.0 | 18.4 | 20.4 | 25.1 | 27.5 |
| 50 | 28.6 | 15.5 | 17.0 | 21.2 | 23.4 |
| 55 | 24.4 | 12.8 | 13.8 | 17.3 | 19.5 |
| 60 | 20.5 | 11.0 | 11.2 | 13.8 | 15.9 |
| 65 | 16.9 | 8.8 | 8.8 | 10.9 | 13.2 |
| 70 | 13.6 | 6.6 | 6.6 | 8.3 | 10.4 |
| 75 | 10.7 | 4.7 | 4.7 | 6.1 | 8.0 |
| 80 | 8.1 | 3.1 | 3.1 | 4.2 | 6.1 |
*Normal values are from 1988 United States life tables for the general population.
Frankel grades:
- A "Complete" — total motor and sensory loss
- B "Sensory only" — sensory sparing
- C "Motor useless" — motor sparing of no functional value
- D "Motor useful" — motor sparing of functional value
- E "Recovery" — no functional deficit
Although it is right to be optimistic about the future of these patients, their injuries can make a devastating change to their lives. In many cases the injuries need not have happened. For example, a high proportion of road traffic accidents is caused by alcohol consumption, high speeds, and dangerous driving, motorcyclists being particularly vulnerable. Ignorance of the danger of diving into shallow water results in many injuries to the cervical spine. Failure to take simple precautions in the home, such as ensuring that stairs are adequately lit at night for the elderly, may result in falls with cervical hyperextension injuries. Carelessness in contact sports can lead to serious injury. Recognition of this fact has led responsible authorities such as the Rugby Football Union to modify the laws of the game and issue advice on how it can be made safer, but much more could be done in other aspects of accident prevention, for instance in horse riding.
Finally, those who work with patients with spinal cord injuries are often impressed by the surprisingly high quality of life possible after injury. Many achieve a remarkable degree of independence, earn their own living, choose to marry, have children, and participate fully in family life. They may indeed have special qualities because they have successfully come to terms with their disability, and many will make a valuable contribution to society.
![]() Attention! Many injuries are preventable:
Attention! Many injuries are preventable:
- Road traffic accidents associated with alcohol consumption and dangerous driving
- Diving into shallow water, resulting in tetraplegia
- Contact sports, e.g., rugby
- Some injuries are made worse by mishandling
See also
- At the accident:
- History and epidemiology of spinal cord injury
- Spinal injuries management at the scene of the accident
- Evacuation and initial management at hospital:
- Evacuation and transfer to hospital of patients with spinal cord injuries
- Initial management of patients with spinal cord injuries at the receiving hospital
- Neurological assessment of patients with spinal cord injuries
- Spinal shock after severe spinal cord injury
- Partial spinal cord injury syndromes
- Radiological investigations:
- Initial radiography of patients with spinal cord injuries
- Cervical injuries
- Thoracic and lumbar injuries
- Early management and complications of spinal cord injuries — I:
- Respiratory complications
- Cardiovascular complications
- Prophylaxis against thromboembolism
- Initial bladder management
- The gastrointestinal tract
- Use of steroids and antibiotics
- The skin and pressure areas
- Care of the joints and limbs
- Later analgesia
- Trauma re-evaluation
- Early management and complications of spinal cord injuries — II:
- The anatomy of spinal cord injury
- The spinal injury (cervical, thoracic and lumbar spine)
- Transfer to a spinal injuries unit
- Medical management in the spinal injuries unit:
- The cervical spine injuries
- The cervicothoracic junction injuries
- Thoracic injuries
- Thoracolumbar and lumbar injuries
- Deep vein thrombosis and pulmonary embolism
- Autonomic dysreflexia
- Biochemical disturbances
- Para-articular heterotopic ossification
- Spasticity
- Contractures
- Pressure sores
- Urological management of patients with spinal cord injury:
- Nursing for people with spinal cord lesion:
- Physiotherapy after spinal cord injury:
- Respiratory management
- Mobilisation into a wheelchair
- Rehabilitation
- Recreation
- Incomplete lesions
- Children
- Occupational therapy after spinal cord injury:
- Hand and upper limb management
- Home resettlement
- Activities of daily living
- Communication
- Mobility
- Leisure
- Work
- Social needs of patient and family:
- Transfer of care from hospital to community:
- Education of patients
- Teaching the family and community staff
- Preparation for discharge from hospital
- Easing transfer from hospital to community
- Travel and holidays
- Follow-up
- Later management and complications after spinal cord injury — I:
- Late spinal instability and spinal deformity
- Pathological fractures
- Post-traumatic syringomyelia (syrinx, cystic myelopathy)
- Pain
- Sexual function
- Later management and complications after spinal cord injury — II:
- Later respiratory management of high tetraplegia
- Psychological factors
- The hand in tetraplegia
- Functional electrical stimulation
- Ageing with spinal cord injury
- Prognosis
- Spinal cord injury in the developing world: