Early management and complications of spinal cord injuries — II
The anatomy of spinal cord injury
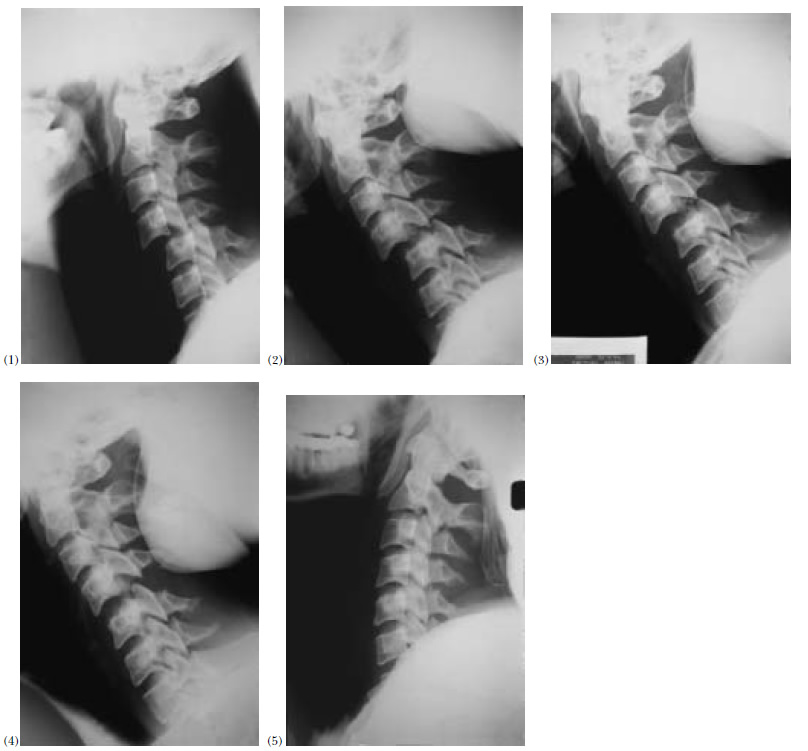
The radiographic appearances of the spine after injury are not a reliable guide to the severity of spinal cord damage. They represent the final or “recoil” position of the vertebrae and do not necessarily indicate the forces generated in the injury. The spinal cord ends at the lower border of the first lumbar vertebra in adults, the remainder of the spinal canal being occupied by the nerve roots of the cauda equina. There is greater room for the neural structures in the cervical and lumbar canals, but in the thoracic region the spinal cord diameter and that of the neural canal more nearly approximate. The blood supply of the cervical spinal cord is good, whereas that of the thoracic cord, especially at its midpoint, is relatively poor. These factors may explain the greater preponderance of complete lesions seen after injuries to the thoracic spine. The initial injury is mechanical, but there is usually an early ischaemic lesion that may rapidly progress to cord necrosis. Extension of this, often many segments below the level of the lesion, accounts for the observation that on occasion patients have lower motor neurone or flaccid paralysis when upper motor neurone or spastic paralysis would have been expected from the site of the bony injury. Because of the potential for regeneration of peripheral nerves, neurological recovery is unpredictable in lesions of the cauda equina.
The spinal injury
Treatment should be aimed at stabilising the spine to avoid further damage by movement and also to relieve cord compression.
The cervical spine injury
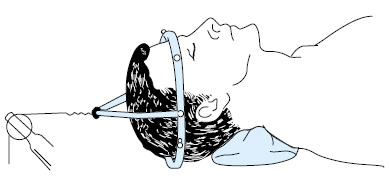
Patients with injuries of the cervical spine should initially be managed by skeletal traction. Applied through skull calipers, traction is aimed at reducing any fracture or dislocation, relieving pressure on the cord in the case of burst fractures, and splinting the spine.
Of the various skull calipers available, spring-loaded types such as the Gardner-Wells are the most suitable for inserting in the emergency department. Local anaesthetic is infiltrated into the scalp down to the periosteum about 2.5 cm above the pinna at the site of the maximum bitemporal diameter, and the caliper is then screwed into the scalp to grip the outer table of the skull. No incisions need be made, and the spring loading of one of the screws determines when the correct tension has been reached. The University of Virginia caliper is similar in action and easily applied. The Cone caliper is satisfactory but requires small scalp incisions and the drilling of 1 mm impressions in the outer table of the skull. Insertion too far anteriorly interferes with temporalis function and causes trismus. The Crutchfield caliper is no longer recommended because of the high incidence of complications.
Skull traction used:
- To reduce dislocation
- To relieve pressure on spinal cord in case of burst fractures
- To splint the spine
When the upper cervical spine is injured less traction is required for reduction and stabilisation. Usually 1–2 kg is enough for stabilisation; if more weight is used overdistraction at the site of injury may cause neurological deterioration. Specific injuries of the upper cervical spine and the cervicothoracic junction are discussed in chapter 6.
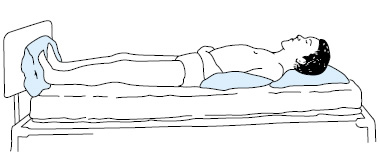
A traction force of 3–5 kg is normally applied to the calipers in fractures of the lower cervical spine without dislocation. A neck roll (not a sandbag) should be placed behind the neck to maintain the normal cervical lordosis. Pressure sores of the scalp in the occipital region are common, and care must be taken to cushion the occiput when positioning the patient. When necessary this can be achieved by using a suitably covered fluid-filled plastic bag, having ensured that there is no matted hair that could act as a source of pressure. If the spine is dislocated reduction can usually be achieved by increasing the weight by about 4 kg every 30 minutes (sometimes up to a total of 25 kg) with the neck in flexion until the facets are disengaged. The neck is then extended and the traction decreased to maintenance weight. The patient must be examined neurologically before each increment, and the traction force must be reduced immediately if the neurology deteriorates.
Manipulation under general anaesthesia is an alternative method of reduction, but, although complete neurological recovery has been reported after this procedure, there have been adverse effects in some patients and manipulation should only be attempted by specialists. Use of an image intensifier may facilitate such reductions.
Halo traction is a useful alternative to skull calipers, particularly in patients with incomplete tetraplegia, and conversion to a halo brace permits early mobilisation.
Skull traction is a satisfactory treatment for unstable injuries of the cervical spine in the early stages, but when the spinal cord lesion is incomplete, early operative fusion may be indicated to prevent further neurological damage. The decision to operate may sometimes be made before the patient is transferred to the spinal injuries unit, and if so the spinal unit should be consulted and management planned jointly.
Another indication for operation is an open wound, such as that following a gunshot or stab injury. Exploration or debridement should be performed.
Skull traction is unnecessary for patients with cervical spondylosis who sustain a hyperextension injury with tetraplegia but have no fracture or dislocation. In these circumstances the patient should be nursed with the head in slight flexion but otherwise free from restriction.
The thoracic and lumbar spine injury
flexion-rotation forces. Conservative treatment for injuries associated with cord damage is designed to minimise spinal movement, and to support the patient to maintain the correct posture. In practice a pillow under the lumbar spine to preserve normal lordosis is sometimes used. Dislocations of the thoracic and lumbar spine may sometimes be reduced by this technique of “postural reduction”. However, internal fixation is recommended in some patients with unstable fracture- dislocations to prevent further cord or nerve root damage, correct deformity, and facilitate nursing. As yet there is no convincing evidence that internal fixation aids neurological recovery.
Transfer to a spinal injuries unit
In the United Kingdom, there are only 11 spinal injuries units and most patients will be admitted to a district general hospital for their initial treatment. As soon as spinal cord injury is diagnosed or suspected the nearest spinal injuries unit should be contacted. Immediate transfer is ideal, as management in an acute specialised unit is associated with reduced mortality, increased neurological recovery, shorter length of stay and reduced cost of care, compared to treatment in a non- specialised centre. The objects of management are to prevent further spinal cord damage by appropriate reduction and stabilisation of the spine, to prevent secondary neuronal injury, and to prevent medical complications.
Objects of early transfer to a spinal injuries unit:
- To prevent further spinal cord damage by reduction and stabilisation of spine
- To prevent secondary neuronal injury
- To prevent medical complications
- To expedite all aspects of rehabilitation
The choice between immediate or early transfer will depend on the general condition of the patient and also on the intensive care facilities available. Unfortunately, some patients will not be fit enough for immediate transfer because of multiple injuries or severe respiratory impairment. In such cases it is advisable to consult, and perhaps arrange a visit by, a spinal injuries consultant. Transfer to a spinal injuries centre is most easily accomplished by means of a Stryker frame, which can be fitted with a constant tension device for skull traction. The RAF pattern turning frame is similarly equipped and was specifically developed for use by the Royal Air Force. In civilian practice, studies have shown that patients can be safely transferred from emergency departments using the standard techniques for cervical immobilisation described earlier. Tetraplegic patients should be accompanied by a suitably experienced doctor with anaesthetic skills, who can quickly intubate the patient if respiratory difficulty ensues. Transfer by helicopter is often the ideal and is advisable if the patient has to travel a long distance.
Delay in transfer to spinal injuries unit if:
- Patient unfit to transfer:
- multiple injuries
- need for emergency surgery
- severe respiratory impairment
- cardiorespiratory instability
- Consider visit by spinal injuries consultant
See also
- At the accident:
- History and epidemiology of spinal cord injury
- Spinal injuries management at the scene of the accident
- Evacuation and initial management at hospital:
- Evacuation and transfer to hospital of patients with spinal cord injuries
- Initial management of patients with spinal cord injuries at the receiving hospital
- Neurological assessment of patients with spinal cord injuries
- Spinal shock after severe spinal cord injury
- Partial spinal cord injury syndromes
- Radiological investigations:
- Initial radiography of patients with spinal cord injuries
- Cervical injuries
- Thoracic and lumbar injuries
- Early management and complications of spinal cord injuries — I:
- Respiratory complications
- Cardiovascular complications
- Prophylaxis against thromboembolism
- Initial bladder management
- The gastrointestinal tract
- Use of steroids and antibiotics
- The skin and pressure areas
- Care of the joints and limbs
- Later analgesia
- Trauma re-evaluation
- Early management and complications of spinal cord injuries — II:
- The anatomy of spinal cord injury
- The spinal injury (cervical, thoracic and lumbar spine)
- Transfer to a spinal injuries unit
- Medical management in the spinal injuries unit:
- The cervical spine injuries
- The cervicothoracic junction injuries
- Thoracic injuries
- Thoracolumbar and lumbar injuries
- Deep vein thrombosis and pulmonary embolism
- Autonomic dysreflexia
- Biochemical disturbances
- Para-articular heterotopic ossification
- Spasticity
- Contractures
- Pressure sores
- Urological management of patients with spinal cord injury:
- Nursing for people with spinal cord lesion:
- Physiotherapy after spinal cord injury:
- Respiratory management
- Mobilisation into a wheelchair
- Rehabilitation
- Recreation
- Incomplete lesions
- Children
- Occupational therapy after spinal cord injury:
- Hand and upper limb management
- Home resettlement
- Activities of daily living
- Communication
- Mobility
- Leisure
- Work
- Social needs of patient and family:
- Transfer of care from hospital to community:
- Education of patients
- Teaching the family and community staff
- Preparation for discharge from hospital
- Easing transfer from hospital to community
- Travel and holidays
- Follow-up
- Later management and complications after spinal cord injury — I:
- Late spinal instability and spinal deformity
- Pathological fractures
- Post-traumatic syringomyelia (syrinx, cystic myelopathy)
- Pain
- Sexual function
- Later management and complications after spinal cord injury — II:
- Later respiratory management of high tetraplegia
- Psychological factors
- The hand in tetraplegia
- Functional electrical stimulation
- Ageing with spinal cord injury
- Prognosis
- Spinal cord injury in the developing world: