Carpal tunnel syndrome
Understanding Carpal Tunnel Syndrome (CTS)
Carpal Tunnel Syndrome (CTS) is a common neurological condition that occurs when the median nerve, one of the major nerves to the hand, is compressed or squeezed as it passes through the carpal tunnel at the wrist. The carpal tunnel is a narrow, rigid passageway formed by the carpal bones at the base of the hand and the transverse carpal ligament (flexor retinaculum) across the top of the wrist.
Definition and Anatomy
The median nerve provides sensation (feeling) to the palm side of the thumb, index finger, middle finger, and half of the ring finger. It also innervates some of the small muscles in the hand at the base of the thumb (thenar muscles), which are responsible for thumb movement and opposition.
Any condition that causes swelling or reduces the space within the carpal tunnel can put pressure on the median nerve, leading to the symptoms of CTS.
Common Causes and Risk Factors
While often associated with repetitive hand and wrist motions, CTS can be caused or exacerbated by a variety of factors:
- Repetitive Hand/Wrist Use: Activities involving prolonged or repetitive flexion and extension of the wrist, or forceful gripping. This is why it is often seen in individuals who work extensively with computers (e.g., using a mouse for long periods), assembly line workers, musicians, or those using vibrating tools.
- Anatomical Factors:
- A congenitally smaller carpal tunnel.
- Wrist fractures or dislocations that alter the tunnel's anatomy.
- Arthritis (rheumatoid arthritis, osteoarthritis) causing inflammation and swelling of wrist joint structures.
- Medical Conditions:
- Diabetes Mellitus: Increased risk of nerve damage.
- Thyroid Dysfunction (Hypothyroidism): Can cause fluid retention and tissue swelling.
- Rheumatoid Arthritis and other Inflammatory Arthropathies.
- Fluid Retention: During pregnancy or menopause.
- Obesity.
- Kidney Failure and Dialysis.
- Acromegaly.
- Tumors or Cysts: Ganglion cysts or other masses within or near the carpal tunnel.
- Positional Factors: Prolonged wrist flexion or extension during sleep.
- Genetic Predisposition.
Symptoms of Carpal Tunnel Syndrome
Typical signs and symptoms of Carpal Tunnel Syndrome include:
- Pain, Numbness, and Tingling (Paresthesias): Primarily affecting the thumb, index finger, middle finger, and the radial half (thumb side) of the ring finger. These symptoms are often more pronounced at night, frequently waking the patient from sleep. Shaking the hand often provides temporary relief ("flick sign").
- Sensation of Swelling: Patients may feel a sensation of swelling or fullness in the hand and wrist, even if no visible swelling is present.
- Weakness in the Hand: Difficulty with gripping objects, dropping things, or weakness in the thumb muscles (thenar muscles), particularly for fine motor tasks like buttoning clothes.
- Radiating Pain: Pain may radiate up the forearm from the wrist.
- Clumsiness: Difficulty with tasks requiring manual dexterity.
Long-Term Complications if Untreated
With a long course of untreated or inadequately managed Carpal Tunnel Syndrome, more severe and potentially irreversible complications can develop:
- Thenar Muscle Atrophy: Wasting or shrinkage of the muscles at the base of the thumb, leading to persistent weakness and loss of thumb function.
- Persistent Numbness and Sensory Loss: Permanent loss of sensation in the affected fingers.
- Osteoporosis in the Phalanges: Rarely, in very chronic and severe cases, osteoporosis (bone thinning) in the bones of the fingers of the affected hand may develop, sometimes in combination with a spasm of blood vessels (vasomotor changes) and persistent burning pains (complex regional pain syndrome - CRPS - though this is a distinct and more complex entity).
Diagnosis of Carpal Tunnel Syndrome
The diagnosis of Carpal Tunnel Syndrome is primarily clinical, based on the patient's symptoms and physical examination findings, often supplemented by electrodiagnostic studies.
Clinical Examination and Provocative Tests
The cause of this condition is established as a result of a thorough examination of the patient and a detailed study of their medical history, occupational activities, and lifestyle characteristics. Typical muscle-tonic symptoms at the level of the forearm of the affected hand may be revealed. Often, the initial diagnosis of carpal tunnel syndrome is based on the neurological examination and specific provocative tests:
- Tinel's Sign: Gently tapping over the median nerve at the wrist. A positive sign elicits tingling or shock-like sensations in the median nerve distribution (thumb, index, middle, and radial half of ring finger).
- Phalen's Maneuver (Wrist Flexion Test): Holding the wrist in complete flexion for 30-60 seconds. A positive sign reproduces or worsens paresthesias in the median nerve distribution.
- Reverse Phalen's Maneuver (Wrist Extension Test): Holding the wrist in extension.
- Carpal Compression Test (Durkan's Test): Applying direct pressure over the carpal tunnel for up to 30 seconds. Reproduction of symptoms is a positive sign.
- Sensory Testing: Assessing light touch, pinprick sensation, and two-point discrimination in the median nerve distribution.
- Motor Testing: Assessing strength of thumb abduction (abductor pollicis brevis muscle) and opposition. Looking for thenar muscle atrophy in advanced cases.
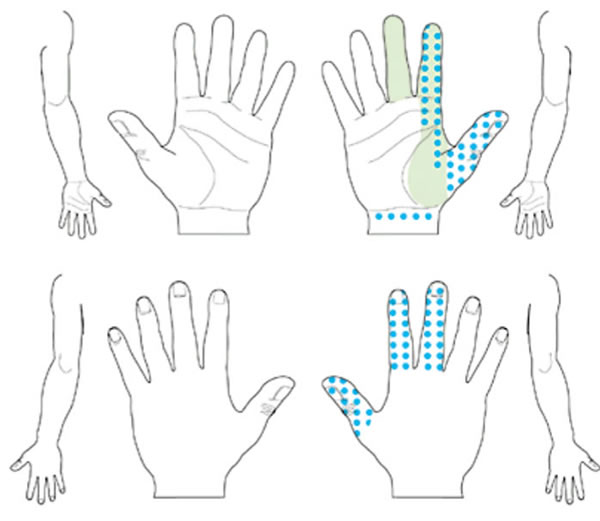
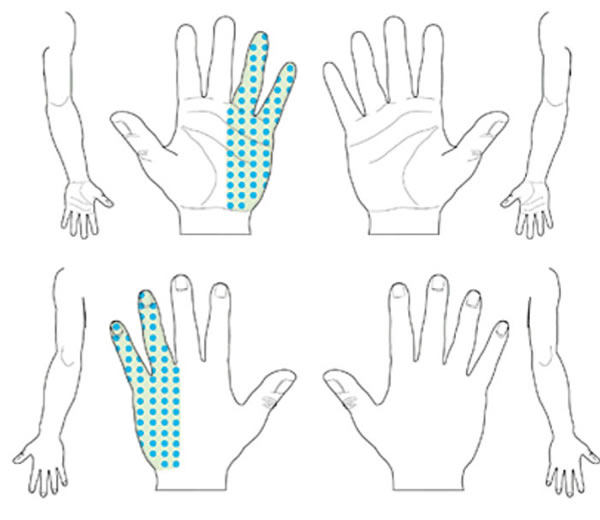
Damage or compression of the median nerve, as in Carpal Tunnel Syndrome (sometimes referred to as median nerve neuritis in this context), typically causes sensory impairment (numbness, tingling, pain) in the thumb (finger I), index finger (II), middle finger (III), and the radial half of the ring finger (IV).
Katz Hand Diagram
Patients can use the **Katz hand diagram** to mark the specific location and nature of their symptoms (pain, numbness, tingling, etc.) on a drawing of the hand. These completed charts can then be classified by the physician as representing a "classic," "probable," "possible," or "unlikely/uncharacteristic" pattern for Carpal Tunnel Syndrome, aiding in diagnostic accuracy.
- Classic Pattern: Symptoms (numbness, pain, tingling) affect at least two of the first three fingers (thumb, index, middle). The classic pattern allows for symptoms in the fourth and fifth fingers (though primarily the radial half of the fourth), wrist pain, and radiation of pain above the wrist, but critically, it *does not* allow for symptoms confined solely to the ulnar aspect (little finger side) of the hand or the dorsum (back) of the hand (except sometimes the fingertips).
- Probable Pattern: Similar symptom distribution as the classic pattern, but symptoms may affect only one of the first three fingers. Symptoms on the ulnar surface of the hand and palm (fifth finger, ulnar half of fourth) are typically excluded from this definition if they are the *only* symptoms.
- Atypical (Unlikely) Pattern: Symptoms are present but do not involve the first, second, or third fingers at all, making CTS less likely.
The classic Katz hand diagram pattern for carpal tunnel syndrome shows symptoms such as numbness, pain, and tingling affecting at least two of the first three digits (thumb, index, middle finger). Symptoms may extend to the fourth/fifth fingers or wrist/forearm, but symptoms exclusively on the ulnar hand or dorsum are not typical.
A "probable" Katz hand diagram pattern for carpal tunnel syndrome involves a similar set of symptoms (numbness, pain, tingling) as the classic case, but may affect only one of the first three digits (thumb, index, or middle finger). Symptoms are generally absent from the ulnar surface of the hand and palm.
Electrodiagnostic Studies (EMG/NCS)
Electromyography (EMG) and Nerve Conduction Studies (NCS/ENG) are objective tests that can confirm median nerve compression at the wrist and assess its severity. They can also help differentiate CTS from other conditions that cause similar symptoms, such as cervical radiculopathy (compression of a nerve root in the neck by an affected intervertebral disc, which can also cause pain and numbness in the upper limb) or other peripheral neuropathies.
NCS typically show:
- Prolonged distal motor latency of the median nerve across the carpal tunnel.
- Slowed sensory nerve conduction velocity across the wrist.
- Reduced amplitude of sensory nerve action potentials (SNAPs) or compound muscle action potentials (CMAPs) in more severe cases.
EMG may show signs of denervation in the thenar muscles in advanced CTS.
Imaging Studies
- Ultrasound: High-resolution ultrasound can visualize the median nerve at the wrist, showing swelling or flattening of the nerve, and can assess the contents of the carpal tunnel. It is increasingly used as a diagnostic tool.
- MRI: Not routinely needed for CTS diagnosis but may be used if a tumor, cyst, or other structural abnormality within the carpal tunnel is suspected, or if the diagnosis is unclear.
Treatment of Carpal Tunnel Syndrome
After a specialist establishes an accurate diagnosis, treatment for Carpal Tunnel Syndrome is determined based on the severity of the symptoms and the impact on the patient's daily life. Options range from conservative measures to surgical intervention if conservative therapy fails to provide positive effects.
Conservative Management
This is typically the first line of treatment for mild to moderate CTS.
- Wrist Splinting: Wearing a neutral position wrist splint, especially at night, helps to keep the wrist straight, reducing pressure on the median nerve and alleviating nocturnal symptoms. A prophylactic wrist brace and pad with a roller can also relieve stress on the median nerve and ligaments in the wrist joint.
- Activity Modification: Avoiding or modifying activities that exacerbate symptoms (e.g., repetitive wrist movements, forceful gripping, prolonged wrist flexion/extension). Ergonomic adjustments at the workplace can be beneficial.
- Ice Application: Applying ice packs to the wrist can help reduce inflammation and pain in some cases.
- Exercises: Nerve gliding exercises and tendon gliding exercises may help improve median nerve mobility within the carpal tunnel.
Elimination of soreness and tingling, along with restoration of sensitivity in the fingers during the treatment of median nerve neuritis associated with carpal tunnel syndrome, is often accelerated with the application of targeted physiotherapy.
In the comprehensive treatment of median nerve neuritis (Carpal Tunnel Syndrome), various physical therapy modalities are employed to accelerate the elimination of soreness and tingling, and to aid in the restoration of normal sensitivity in the affected fingers.
Pharmacological Treatment
- Non-Steroidal Anti-Inflammatory Drugs (NSAIDs): Oral NSAIDs (e.g., ibuprofen, naproxen) may help relieve pain and inflammation, particularly if synovitis (inflammation of tendon sheaths) is present.
- Analgesics: Simple pain relievers like acetaminophen.
- Oral Corticosteroids (Hormones): A short course of oral steroids may be considered for acute, severe symptoms to reduce inflammation quickly, but long-term use is not recommended due to side effects.
- Medications for neuropathic pain (e.g., gabapentin, pregabalin) if pain is a prominent feature.
Therapeutic Injections
- Corticosteroid Injections: Injection of a corticosteroid medication directly into or near the carpal tunnel can provide significant, though often temporary, relief from symptoms by reducing inflammation and swelling around the median nerve. This can also be a diagnostic aid.
Manual and Physical Therapies
- Manual Therapy: Techniques performed by a qualified therapist, such as soft tissue mobilization, joint mobilization (articular technique), and specific nerve mobilization techniques (radicular technique for referred symptoms, though CTS is peripheral), may help alleviate symptoms.
- Physiotherapy: Modalities like ultrasound therapy (UHF - though UHF usually refers to Ultra High Frequency diathermy rather than therapeutic ultrasound for CTS), iontophoresis, or phonophoresis (using ultrasound to deliver medication through the skin), Cold Laser Therapy (CMT - likely Cold Laser or Low-Level Laser Therapy), may be used to reduce pain and inflammation.
- Acupuncture: Some patients find acupuncture helpful for pain relief.
Surgical Treatment (Carpal Tunnel Release)
Surgical intervention is considered if:
- Conservative therapy has failed to provide adequate relief after several weeks or months.
- Symptoms are severe and persistent.
- There is evidence of thenar muscle atrophy or significant motor weakness.
- Electrodiagnostic studies show moderate to severe median nerve compression.
The surgical procedure is called **carpal tunnel release**. It involves cutting the transverse carpal ligament to relieve pressure on the median nerve and increase the volume of the carpal tunnel. This can be done through:
- Open Carpal Tunnel Release: Involves a small incision on the palm side of the wrist.
- Endoscopic Carpal Tunnel Release: Uses one or two smaller incisions and an endoscope (a small camera) to visualize and cut the ligament. This may allow for a quicker recovery and less postoperative pain for some patients.
Surgery is generally effective in relieving symptoms, especially pain and paresthesias. Recovery of strength and sensation can take longer if nerve damage was severe or long-standing.
Differential Diagnosis of Hand Pain and Numbness
Symptoms of Carpal Tunnel Syndrome can mimic other conditions. A thorough differential diagnosis is important:
| Condition | Key Differentiating Features |
|---|---|
| Carpal Tunnel Syndrome (CTS) | Pain, numbness, tingling in median nerve distribution (thumb, index, middle, radial half of ring finger), often worse at night. Positive Tinel's, Phalen's. EMG/NCS shows median neuropathy at wrist. |
| Cervical Radiculopathy (C6 or C7 Nerve Root) | Neck pain often present, radiating pain/numbness into arm/hand following a dermatomal pattern (C6: thumb/index; C7: middle finger). Weakness in corresponding myotomes. Reflex changes in arm. Symptoms may worsen with neck movements. Neck MRI diagnostic. |
| Pronator Teres Syndrome | Median nerve compression in the proximal forearm by pronator teres muscle. Aching pain in forearm, sensory loss similar to CTS but often spares nocturnal symptoms and may have tenderness over pronator muscle. Phalen's/Tinel's at wrist usually negative. |
| Thoracic Outlet Syndrome (Neurogenic) | Compression of brachial plexus. Pain, numbness, tingling often in ulnar distribution (C8-T1, little/ring fingers, medial forearm) but can be variable. Symptoms worsen with arm elevation. |
| Ulnar Neuropathy (Cubital Tunnel Syndrome or Guyon's Canal) | Numbness/tingling in little finger and ulnar half of ring finger, weakness of intrinsic hand muscles. Tinel's at elbow (cubital tunnel) or wrist (Guyon's canal). |
| Peripheral Polyneuropathy (e.g., Diabetic) | Usually symmetrical, distal "stocking-glove" sensory loss, pain, and weakness affecting both hands and feet. |
| De Quervain's Tenosynovitis | Pain and tenderness at the base of the thumb on the radial side of the wrist, related to inflammation of thumb tendons. Positive Finkelstein's test. No numbness/tingling typically. |
| Wrist Arthritis (Osteoarthritis or Rheumatoid) | Joint pain, stiffness, swelling in the wrist. Morning stiffness common in RA. X-rays show joint changes. |
Prevention Strategies for Carpal Tunnel Syndrome
While not all cases are preventable, certain measures can reduce risk or alleviate early symptoms:
- Ergonomics: Proper workstation setup (keyboard, mouse position, chair height) to maintain neutral wrist posture.
- Regular Breaks and Stretching: Taking frequent short breaks from repetitive hand/wrist activities. Performing wrist and hand stretching exercises.
- Maintain Neutral Wrist Posture: Avoid prolonged extreme flexion or extension of the wrist.
- Reduce Forceful Gripping: Use a lighter grip when possible.
- Keep Hands Warm: Cold can exacerbate symptoms for some individuals.
- Manage Underlying Medical Conditions: Good control of diabetes, thyroid disorders, or arthritis.
- Maintain a Healthy Weight.
When to Consult a Specialist (Neurologist, Hand Surgeon)
It is advisable to consult a physician, neurologist, or hand surgeon if:
- Symptoms of pain, numbness, or tingling in the hand/fingers are persistent, recurrent, or worsening.
- Symptoms interfere with sleep or daily activities.
- There is noticeable weakness in the hand or thumb, or dropping objects.
- Conservative home measures (rest, splinting, activity modification) do not provide relief.
- Thenar muscle atrophy is observed.
Early diagnosis and appropriate management can prevent progression of nerve damage and lead to better outcomes.
References
- American Academy of Orthopaedic Surgeons (AAOS). Carpal Tunnel Syndrome. OrthoInfo. Rosemont, IL: AAOS; Updated February 2023.
- Katz JN, Gelberman RH, Wright EA, Lew RA, Frauenthal A. The carpal tunnel syndrome: diagnostic utility of the history and physical examination findings. Ann Intern Med. 1990 Sep 1;113(5):337-41. (Katz Hand Diagram origin)
- Graham B. The value added by electrodiagnostic testing in the diagnosis of carpal tunnel syndrome. J Bone Joint Surg Am. 2008 Dec;90(12):2587-93.
- Padua L, Coraci D, Erra C, et al. Carpal tunnel syndrome: clinical features, diagnosis, and management. Lancet Neurol. 2016 Nov;15(12):1273-1284.
- Middleton WD, Rybicki FJ, Sardiwalla II, et al. ACR Appropriateness Criteria® Carpal Tunnel Syndrome. J Am Coll Radiol. 2017 May;14(5S):S62-S69.
- Aroori S, Spence RA. Carpal tunnel syndrome. Ulster Med J. 2008 Jan;77(1):6-17.
- Keith MW, Masear V, Chung K, et al. Diagnosis of carpal tunnel syndrome. J Am Acad Orthop Surg. 2009 Jun;17(6):389-96.
- Urbaniak JR. Carpal tunnel syndrome. South Med J. 1990 Feb;83(2):204-9.
See also
- Anatomy of the nervous system
- Spinal disc herniation
- Pain in the arm and neck (trauma, cervical radiculopathy)
- The eyeball and the visual pathway:
- Anatomy of the eye and physiology of vision
- The visual pathway and its disorders
- Eye structures and visual disturbances that occur when they are affected
- Retina and optic disc, visual impairment when they are affected
- Impaired movement of the eyeballs
- Nystagmus and conditions resembling nystagmus
- Dry Eye Syndrome
- Optic nerve and retina:
- Compression neuropathy of the optic nerve
- Edema of the optic disc (papilledema)
- Ischemic neuropathy of the optic nerve
- Meningioma of the optic nerve sheath
- Optic nerve atrophy
- Optic neuritis in adults
- Optic neuritis in children
- Opto-chiasmal arachnoiditis
- Pseudo-edema of the optic disc (pseudopapilledema)
- Toxic and nutritional optic neuropathy
- Neuropathies and neuralgia:
- Diabetic, alcoholic, toxic and small fiber sensory neuropathy (SFSN)
- Facial nerve neuritis (Bell's palsy, post-traumatic neuropathy)
- Fibular (peroneal) nerve neuropathy
- Median nerve neuropathy
- Neuralgia (intercostal, occipital, facial, glossopharyngeal, trigeminal, metatarsal)
- Post-traumatic neuropathies
- Post-traumatic trigeminal neuropathy
- Post-traumatic sciatic nerve neuropathy
- Radial nerve neuropathy
- Tibial nerve neuropathy
- Trigeminal neuralgia
- Ulnar nerve neuropathy
- Tumors (neoplasms) of the peripheral nerves and autonomic nervous system (neuroma, sarcomatosis, melanoma, neurofibromatosis, Recklinghausen's disease)
- Carpal tunnel syndrome
- Ulnar nerve compression in the cubital canal