Orchitis, didymitis, testicular inflammation
- Understanding Orchitis and Epididymo-orchitis (Testicular Inflammation)
- Symptoms of Acute and Chronic Orchitis/Epididymo-orchitis
- Diagnosis of Orchitis and Epididymo-orchitis
- Treatment of Orchitis and Epididymo-orchitis
- Potential Complications and Long-Term Sequelae
- Differential Diagnosis of Acute Scrotal Pain and Swelling
- Prevention Strategies
- When to Consult a Urologist
- References
Understanding Orchitis and Epididymo-orchitis (Testicular Inflammation)
Orchitis is an inflammation of one or both testicles (testes). It is often associated with inflammation of the epididymis (a coiled tube located at the back of the testicle that stores and carries sperm), a condition known as epididymitis. When both the testicle and epididymis are inflamed, the condition is termed epididymo-orchitis. These conditions can cause significant pain and swelling in the scrotum.
Definitions and Common Causes
As a rule, orchitis develops as a complication of various underlying conditions, including:
- Systemic Infectious Diseases: Mumps is a classic cause of viral orchitis, especially in post-pubertal males. Other viral infections can also be implicated.
- Diseases of the Genitourinary System: Infections can spread from other parts of the male reproductive or urinary system, such as:
- Urethritis (inflammation of the urethra)
- Prostatitis (inflammation of the prostate gland)
- Epididymitis (which frequently precedes or accompanies orchitis)
- Urinary tract infections (UTIs)
- Sexually Transmitted Infections (STIs): Pathogens causing STIs are a common cause of epididymitis and subsequent orchitis in sexually active men.
- Testicular Trauma: Injury to the testicle can predispose to inflammation and secondary infection.
- Instrumentation or Surgery: Procedures involving the urethra or bladder can sometimes lead to ascending infection.
Types of Orchitis: Specific vs. Nonspecific
Orchitis can be classified based on the causative agent of the inflammation:
- Specific Orchitis: This type is caused by specific microorganisms responsible for distinct systemic diseases. Examples include orchitis due to:
- *Mycobacterium tuberculosis* (tuberculous orchitis)
- *Treponema pallidum* (syphilitic orchitis)
- *Brucella* species (brucellar orchitis)
- *Actinomyces* species (actinomycotic orchitis)
- Mumps virus (mumps orchitis - technically viral, but often considered separately due to its distinct clinical importance)
- Nonspecific Orchitis: This type is caused by common viruses, bacteria, or protozoa that do not cause a uniquely identifiable systemic disease picture leading to orchitis.
- Bacterial Orchitis: Often results from ascending infection from the urethra or bladder, or hematogenous spread. Common bacteria include *Escherichia coli*, *Klebsiella pneumoniae*, *Pseudomonas aeruginosa*, and staphylococci/streptococci.
- Viral Orchitis (other than mumps): Coxsackievirus, echovirus, varicella-zoster virus can rarely cause orchitis.
In recent times, sexually transmitted infections (STIs) have become a very common cause of epididymitis, which frequently progresses to epididymo-orchitis, particularly in sexually active men. Common STI pathogens include:
- Chlamydia trachomatis
- Neisseria gonorrhoeae (Gonococcus)
- Mycoplasma genitalium
- Ureaplasma urealyticum
- Trichomonas vaginalis (less common as a direct cause of orchitis, but can cause urethritis predisposing to ascending infection)
Symptoms of Acute and Chronic Orchitis/Epididymo-orchitis
Orchitis and epididymo-orchitis are classified as acute or chronic based on the severity of symptoms and the duration of the illness.
The main symptoms of **acute orchitis** (or acute epididymo-orchitis) include:
- Scrotal Pain: The patient typically experiences severe pain in the affected half of the scrotum where the inflammatory process has begun. The pain can be sudden in onset and may radiate to the groin, perineum, lower back (loin), and sacrum.
- Scrotal Swelling and Redness: The affected side of the scrotum enlarges (swells), and the overlying skin becomes erythematous (red), warm to the touch, and smooth due to edema.
- Testicular Tenderness and Enlargement: On palpation, the inflamed testicle (and often the epididymis) is exquisitely tender and palpably enlarged.
- Systemic Symptoms: The patient's general state of health often worsens, with symptoms such as:
- Fever (pyrexia)
- Chills
- Headache
- Nausea
- Malaise
- Urinary Symptoms (if associated urethritis or UTI): Dysuria (painful urination), urinary frequency, urgency, or urethral discharge may be present.
Chronic orchitis may develop after an inadequately treated acute episode or have an insidious onset. Symptoms are generally milder but more persistent than in acute orchitis. They can include chronic testicular pain or discomfort, induration (hardening) or slight enlargement of the testicle, and sometimes recurrent low-grade fevers. Often, chronic orchitis is associated with chronic prostatitis, vesiculitis (seminal vesicle inflammation), or urethritis.
Diagnosis of Orchitis and Epididymo-orchitis
Diagnosing orchitis and epididymo-orchitis involves a thorough clinical evaluation and targeted laboratory and imaging studies:
- Medical History and Physical Examination:
- Detailed history of symptoms (onset, duration, severity of pain, associated urinary or systemic symptoms), sexual history, history of recent infections (e.g., mumps, UTIs), trauma, or urological procedures.
- Physical examination includes inspection and palpation of the scrotum, testes, and epididymides for swelling, tenderness, redness, and warmth. Examination of the prostate may be done if prostatitis is suspected.
- Laboratory Tests:
- Urinalysis (in three portions or midstream clean-catch): To detect pyuria (white blood cells), bacteriuria, and hematuria, which may indicate a urinary tract infection.
- Urine Culture and Sensitivity: To identify bacterial pathogens and guide antibiotic therapy if UTI is present.
- Urethral Smear/Swab (Microscopic Examination and Culture/NAAT): Essential for diagnosing urethritis and identifying STI pathogens like *N. gonorrhoeae* and *C. trachomatis*. PCR diagnostics for genital infections (Chlamydia, Mycoplasma, Ureaplasma, Gonococcus, Trichomonas, etc.) are highly sensitive.
- Complete Blood Count (CBC): May show leukocytosis (elevated white blood cell count) with a left shift, indicating infection.
- Inflammatory Markers: C-reactive protein (CRP) may be elevated.
- Serological Tests: For specific infections if suspected (e.g., mumps IgM/IgG if mumps orchitis is considered, syphilis serology).
- Microscopic Examination of Prostate Secretion and Prostatic Specific Antigen (PSA): If concomitant prostatitis is suspected, especially in older men or with chronic symptoms.
- Imaging Studies:
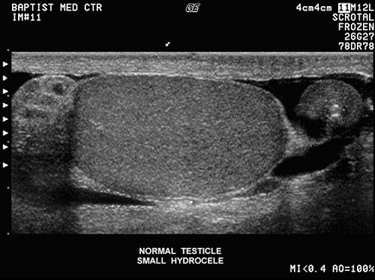
- Scrotal Ultrasound (Doppler Ultrasound): This is the primary imaging modality. It can confirm inflammation of the testicle and/or epididymis (enlargement, increased blood flow on Doppler), detect complications like abscess formation or hydrocele (fluid collection), and importantly, help differentiate epididymo-orchitis from testicular torsion (a surgical emergency characterized by absent or decreased blood flow to the testicle). A normal ultrasound of the scrotum shows homogenous testicular tissue with normal blood flow.
- Ureteroscopy (Rarely for diagnosis of orchitis itself): Ureteroscopy is an endoscopic examination of the ureters and is not typically used for diagnosing orchitis directly but might be part of a broader urological workup if related urinary tract pathology is suspected.
Treatment of Orchitis and Epididymo-orchitis
The treatment of orchitis and epididymo-orchitis requires an integrated approach, focusing on eradicating the infection, alleviating symptoms, treating any concomitant diseases, and eliminating factors contributing to the development of the inflammation.
General Principles and Medical Management
- Antibiotic Therapy: This is the mainstay for bacterial orchitis/epididymo-orchitis. The choice of antibiotic depends on the likely pathogen and patient age/risk factors:
- For STIs (e.g., Chlamydia, Gonorrhea) in sexually active men: Typically a combination like ceftriaxone (intramuscular) plus doxycycline or azithromycin (oral).
- For non-STI bacterial infections (often enteric organisms like *E. coli*), common in older men with BPH or younger prepubertal boys: Fluoroquinolones (e.g., ciprofloxacin, levofloxacin - generally avoided in children if possible), or trimethoprim-sulfamethoxazole.
- Treatment duration is usually 10-14 days or longer.
- Supportive Care:
- Bed Rest and Scrotal Support/Elevation: Helps to reduce pain and swelling. An athletic supporter or towel sling can provide fixation of the scrotum.
- Ice Packs: Applied to the scrotum (wrapped in a cloth) can help reduce swelling and pain.
- Analgesics and Anti-inflammatory Drugs: NSAIDs (e.g., ibuprofen, naproxen) for pain and inflammation. Stronger pain medication may be needed for severe pain.
- Hydration.
- Treatment of Viral Orchitis (e.g., Mumps): Primarily supportive, as antibiotics are ineffective. Pain relief, scrotal support, and rest are key. Antiviral medications are not typically used.
- Local Compresses (Historical/Adjunctive): Alcohol-balsamic compresses were sometimes used locally, but their efficacy is not well-established by modern evidence.
Management of Chronic Forms and Suppuration
- Chronic Orchitis/Epididymo-orchitis: Treatment focuses on identifying and managing any underlying persistent cause (e.g., chronic prostatitis, urethral stricture). Longer courses of antibiotics may be needed. Anti-inflammatory medications and pain management are important. Physiotherapy procedures may be indicated after the acute inflammation has subsided.
- Testicular Abscess (Suppuration of the Testicle): If the testicle develops an abscess (a collection of pus), surgical drainage is usually required. The abscess is opened and washed out. If conservative management with antibiotics and drainage fails to resolve a severe testicular abscess or if the testicle is extensively damaged and non-viable, an **orchiectomy** (surgical removal of the affected testicle) may be necessary to control the infection and prevent further complications.
Potential Complications and Long-Term Sequelae
If orchitis or epididymo-orchitis is not treated promptly or adequately, the disease can become chronic, or lead to significant complications:
- Testicular Atrophy: Inflammation can damage testicular tissue, leading to shrinkage and impaired function of the testicle. This may occur 1-2 months after the acute episode if not properly managed.
- Testicular Abscess Formation.
- Chronic Epididymitis or Orchitis: Persistent pain and inflammation.
- Infertility: Bilateral orchitis, especially mumps orchitis occurring after puberty, or severe epididymo-orchitis can lead to damage to sperm-producing cells or obstruction of the sperm ducts, resulting in a significant decrease in sperm production or quality, potentially causing infertility.
- Scrotal Fistula: Rarely, an abscess can drain spontaneously through the scrotal skin.
- Spread of Inflammation: Inflammation can spread from one testicle to the other if the underlying cause is not addressed.
- Reactive Hydrocele: Fluid collection around the testicle.
Differential Diagnosis of Acute Scrotal Pain and Swelling
Acute scrotal pain and swelling require prompt evaluation to differentiate orchitis/epididymo-orchitis from other serious conditions, particularly testicular torsion:
| Condition | Key Differentiating Features |
|---|---|
| Epididymo-orchitis / Orchitis | Gradual onset of pain and swelling over hours to days; often associated with fever, urinary symptoms (dysuria, frequency, discharge); epididymis tender and swollen initially, then testis. Prehn's sign (elevation of scrotum relieves pain) may be positive (unreliable). Doppler US shows increased blood flow. |
| Testicular Torsion | Sudden, severe onset of unilateral testicular pain, often with nausea/vomiting; testis may be high-riding and transversely oriented; cremasteric reflex usually absent. Doppler US shows absent or decreased blood flow to the testis. **Surgical emergency requiring immediate intervention.** |
| Torsion of Testicular or Epididymal Appendage | Sudden onset of localized pain, often in upper pole of testis or epididymis; "blue dot" sign may be visible through scrotal skin. Doppler US shows normal or increased testicular flow, with a focal avascular or hyperechoic appendage. More common in prepubertal boys. |
| Inguinal Hernia (Incarcerated/Strangulated) | Groin/scrotal swelling, pain, irreducibility. May have signs of bowel obstruction if strangulated. US can help differentiate. |
| Hydrocele (Acute/Reactive) | Fluid collection around testis; usually painless unless acute or infected. Transilluminates. Can be secondary to epididymo-orchitis or torsion. |
| Varicocele (Acute Thrombosis - Rare) | Sudden pain in a pre-existing varicocele. "Bag of worms" palpable. |
| Testicular Tumor with Hemorrhage or Necrosis | Can present with acute pain/swelling. Testicular mass palpable. US is key. Tumor markers (AFP, hCG, LDH) may be elevated. |
| Idiopathic Scrotal Edema | Painless or mildly painful scrotal swelling and redness, often in young boys, without significant testicular or epididymal inflammation. Self-limiting. |
Prevention Strategies
Preventive measures depend on the underlying cause:
- Mumps Vaccination: MMR vaccine significantly reduces the risk of mumps orchitis.
- Safe Sexual Practices: Using condoms and limiting sexual partners can prevent STIs that cause epididymitis/orchitis.
- Prompt Treatment of UTIs and Prostatitis: To prevent ascending infection.
- Avoidance of Testicular Trauma: Using protective gear during sports.
- Good Personal Hygiene.
When to Consult a Urologist
Seek immediate medical attention, preferably from a urologist or in an emergency department, if you experience:
- Sudden onset of severe testicular or scrotal pain.
- Swelling, redness, or warmth of the scrotum.
- Fever or chills associated with scrotal pain.
- Painful urination or urethral discharge.
- Any trauma to the testicles.
Prompt diagnosis and treatment are crucial to relieve pain, eradicate infection, prevent complications like testicular atrophy or infertility, and to rule out surgical emergencies like testicular torsion.
References
- Street EJ, Justice ED, Kopa Z, et al. The 2021 European Association of Urology Guidelines on Sexual and Reproductive Health-Aspects of Male Reproduction and Urological Infections. Eur Urol. 2021;80(5):541-550. (Covers STIs and related infections)
- Luzzi GA, O'Brien TS. Acute epididymitis. BJU Int. 2001 May;87(8):747-55.
- Trojian TH, Lishnak TS, Heiman D. Epididymitis and orchitis: an overview. Am Fam Physician. 2009 Apr 1;79(7):583-7.
- Nickel JC. Prostatitis and related conditions, orchitis, and epididymitis. In: Wein AJ, Kavoussi LR, Partin AW, Peters CA, eds. Campbell-Walsh Urology. 11th ed. Elsevier; 2016:chap 13.
- World Health Organization. Mumps. Accessed [Current Date]. (Information on mumps and its complications).
- Workowski KA, Bachmann LH, Chan PA, et al. Sexually Transmitted Infections Treatment Guidelines, 2021. MMWR Recomm Rep. 2021 Jul 23;70(4):1-187.
- García-Morúa A, Vaes S, Norkobilov A, et al. Mumps Orchitis: A Comprehensive Review. World J Mens Health. 2021 Jan;39(1):41-56.
- Ludwig M. Diagnosis and therapy of acute prostatitis, epididymitis and orchitis. Andrologia. 2008 Apr;40(2):76-80.
See also
- Benign Prostatic Hyperplasia (BPH)
- Cystitis (Bladder Infection)
- Hydrocele (Testicular Fluid Collection)
- Kidney Stones (Urolithiasis)
- Kidney (Urinary) Syndromes & Urinalysis Findings
- Bilirubinuria and Urobilinogenuria
- Cylindruria (Casts in Urine)
- Glucosuria (Glucose in Urine)
- Hematuria (Blood in Urine)
- Hemoglobinuria (Hemoglobin in Urine)
- Ketonuria (Ketone Bodies in Urine)
- Myoglobinuria (Myoglobin in Urine)
- Proteinuria (Protein in Urine)
- Porphyrinuria (Porphyrins in Urine) & Porphyria
- Pyuria (Leukocyturia - WBCs in Urine)
- Orchitis & Epididymo-orchitis (Testicular Inflammation)
- Prostatitis (Prostate Gland Inflammation)
- Pyelonephritis (Kidney Infection)
- Hydronephrosis & Pyonephrosis
- Varicocele (Enlargement of Spermatic Cord Veins)
- Vesiculitis (Seminal Vesicle Inflammation)