Echoencephalography (EhoEG)
Echoencephalography (EhoEG)
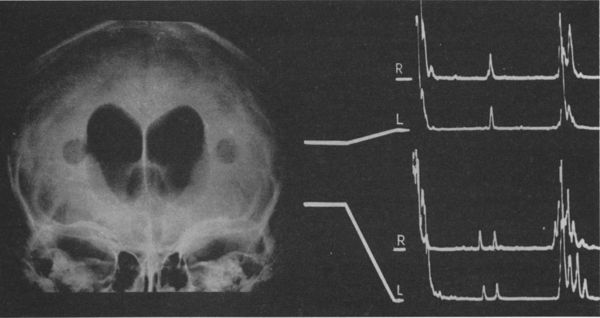
Echoencephalography (EhoEG) is a non-invasive diagnostic ultrasound technique primarily used to assess the position of midline brain structures. It operates by transmitting pulses of ultrasound through the skull and detecting the echoes reflected from interfaces between intracranial structures with different acoustic densities (e.g., scalp, skull bone, meninges, brain tissue, cerebrospinal fluid, blood). While largely superseded by CT and MRI for detailed structural imaging, EhoEG historically played a crucial role and may still have niche applications (e.g., bedside screening, resource-limited settings) due to its portability and lack of ionizing radiation.
Abnormal intracranial formations, such as hematomas, tumors, abscesses, cysts, foci of contusion, or foreign bodies, can also potentially generate echoes if their acoustic properties differ significantly from surrounding tissues.
The M-Echo and Midline Shift
The most significant finding in traditional A-mode EhoEG is the position of the midline echo (M-echo). This prominent echo originates from structures along the brain's midline, like the third ventricle, falx cerebri, or septum pellucidum. By comparing the distance from the transducer to the M-echo on both sides of the head, or by comparing the M-echo position relative to the total skull width, a displacement (shift) of these midline structures can be identified. A physiological asymmetry can allow for a midline shift of up to 2 mm in healthy individuals. A shift exceeding this threshold typically indicates a space-occupying lesion or unilateral swelling causing mass effect.
Clinical Indications
EhoEG has been employed in the diagnostic workup of various conditions, particularly when assessing for mass effect:
- Suspected Intracranial Hematomas (following TBI)
- Brain Tumors or Abscesses (causing midline shift)
- Hydrocephalus (assessment of ventricular size, though less precise than CT/MRI)
- Severe Headaches or Neurological deficits suggesting a mass lesion
- Ischemic stroke, cerebral ischemia (primarily to rule out large hemorrhage with shift)
- Vertebrobasilar insufficiency (VBI) with vertigo symptom (as part of broader assessment)
- Somatoform disorder (autonomic dysfunction) (less common indication)
- Transient ischemic attack (TIA)
- Dizziness (vertigo)
- Tinnitus
- Raised Intracranial pressure (indirect assessment via shift or pulsation changes)
- Headache (when suspecting structural cause)
- Concussion and brain contusion (to assess for complications like hematoma)
- Neck injuries, cervical-cranial syndrome
- Encephalopathy
- Parkinson's disease (not a primary tool)
- Hypophyseal adenoma (MRI is standard; EhoEG limited)
Findings in Traumatic Brain Injury (TBI)
In brain concussion without significant swelling or hematoma, the M-echo displacement typically remains within physiological limits (≤ 2 mm). With focal brain contusion, cerebral edema can cause a progressive M-echo shift towards the intact hemisphere, potentially reaching 2-5 mm, peaking around day 4 post-injury, and gradually resolving over weeks. Sometimes, spike-like signals from small hemorrhages within the contusion may be detected.
EhoEG is particularly valuable for the rapid detection of expanding supratentorial hematomas (epidural or subdural), which can cause significant M-echo shifts (e.g., 6-15 mm or more) relatively early after TBI. Direct echoes from the hematoma-brain interface may sometimes be visualized, appearing as a non-pulsating, high-amplitude signal. Locating the hematoma echo itself can be difficult if it lies within the transducer's "dead zone"; thus, measuring from the contralateral side is often necessary. Scalp swelling or hematoma can complicate measurements by altering the perceived skull surface; careful identification of the inner table echo is crucial.
Limitations and Other Findings
The diagnostic value of EhoEG is reduced for bilateral lesions, posterior fossa pathology, or lesions near the skull base or frontal poles, as these may not produce a significant midline shift detectable via standard temporal windows. In these cases, the absence of midline shift does not rule out significant pathology. While less precise than modern imaging, EhoEG can also provide rough estimates of ventricular size and assess the pulsation amplitude of the M-echo. Increased pulsation may correlate with raised intracranial pressure, while absent pulsation is a grave sign suggesting cessation of cerebral blood flow (in the context of brain death). Modern multi-dimensional or B-mode ultrasound techniques offer more anatomical detail but are also less commonly used for primary diagnosis compared to CT/MRI.
References
- Leksell L. Echo-encephalography. I. Detection of intracranial complications following head injury. Acta Chir Scand. 1955-1956;110(4):301-15. PMID: 13291899.
- White DN. The early development of neurosonology: I. Echoencephalography in adults (A-mode). Ultrasound Med Biol. 1989;15(Suppl 1):51-61. DOI: 10.1016/0301-5629(89)90097-1.
- Schlake HP, Roosen K. A-mode echoencephalography--still a useful tool in the era of CT and MRI? Ultraschall Med. 1994 Aug;15(4):168-75. DOI: 10.1055/s-2007-1004046. PMID: 7974865.
- Uematsu S, Walker AE. A manual of echoencephalography. Baltimore: Williams & Wilkins; 1971.
- Greenberg MS. Handbook of Neurosurgery. 9th ed. Thieme; 2020. (Provides context on diagnostic tools).