Electroencephalography (EEG) in adults and children
What is Electroencephalography (EEG)?
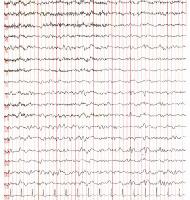
Electroencephalography (EEG) is a non-invasive neurophysiological technique used to record the spontaneous electrical activity of the brain. This activity, often referred to as brain waves, arises from the summed electrical currents generated by large populations of neurons firing within the cerebral cortex. The test is applicable and valuable for both adults and children.
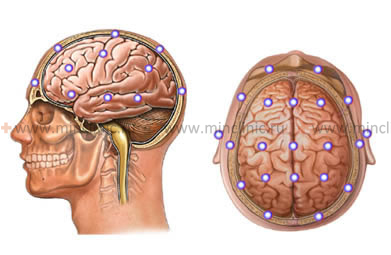
The recording is performed using specialized devices called electroencephalographs. These instruments utilize sensitive electrodes placed on the scalp according to a standardized pattern (commonly the International 10-20 system) to detect the minute electrical potential fluctuations (typically measured in microvolts, µV). Amplifiers within the EEG machine magnify these signals thousands of times, allowing them to be displayed visually on a screen or printed on paper, providing a graphical representation of brain activity over time.
Normal Brain Rhythms on EEG
The EEG of a healthy, awake adult typically shows a predominant rhythm when relaxed with eyes closed, known as the alpha rhythm. This rhythm occurs mainly over the posterior regions of the head and has a frequency of 8-13 Hz (cycles per second) and an amplitude usually around 20-60 µV. Opening the eyes or performing mental tasks typically suppresses or attenuates the alpha rhythm.
Other normal rhythms are also present:
- Beta rhythms (13-30 Hz): Lower amplitude waves, usually seen over the frontal regions or more diffusely during alertness, concentration, or anxiety.
- Theta rhythms (4-7 Hz): Normally present during drowsiness, light sleep, or in young children during wakefulness. Increased theta during wakefulness in adults can sometimes indicate pathology.
- Delta rhythms (0.5-4 Hz): The slowest waves, characteristic of deep sleep in adults. Their presence during wakefulness in adults is generally abnormal and often indicates underlying brain dysfunction or injury.
The EEG pattern changes significantly with the individual's functional state. For instance, transitioning from wakefulness to sleep involves a predictable sequence: disappearance of alpha rhythm, emergence of theta, followed by sleep spindles and K-complexes in stage 2 sleep, and finally the dominance of delta waves in deep sleep (stages 3 and 4). Strong emotional states or sensory stimulation can also alter EEG patterns.
Role of EEG Compared to Imaging
While advanced neuroimaging techniques like Computed Tomography (CT) and Magnetic Resonance Imaging (MRI) excel at visualizing the brain's structure and identifying anatomical lesions (tumors, strokes, bleeding), EEG provides crucial information about brain *function*. It directly measures the real-time electrical activity and is therefore indispensable for diagnosing conditions primarily characterized by abnormal brain function, such as epilepsy. It remains a vital tool for assessing the functional state of the brain, evaluating seizure disorders, monitoring coma depth, assessing encephalopathy, and investigating sleep disorders, complementing rather than being replaced by structural imaging.
Indications and Findings in EEG Tests
The primary and most well-established indication for EEG is the diagnosis and management of epilepsy and seizure disorders. EEG can help classify seizure types, identify the location of seizure onset (focal epilepsy), monitor treatment effectiveness, and contribute to prognostic assessment.
Other important indications include:
- Evaluation of altered consciousness, confusion, or coma.
- Diagnosis and assessment of encephalopathies (diffuse brain dysfunction due to metabolic, toxic, or infectious causes).
- Evaluation of suspected non-epileptic events (to differentiate seizures from psychogenic events or other paroxysmal disorders).
- Assessment of certain sleep disorders (though often polysomnography, which includes EEG, is used).
- Evaluation of specific developmental delays or regression in children.
- Prognostication after cardiac arrest or severe brain injury.
- Confirmation of brain death (requires specific protocols showing electrocerebral inactivity).
It is important to note that EEG is most valuable when performed to answer a specific clinical question. Ordering an EEG for non-specific symptoms like uncomplicated headache without associated neurological signs (such as seizure-like events) is often low-yield. Non-specific findings on such EEGs can sometimes cause unnecessary anxiety for patients or parents and may complicate diagnosis rather than clarify it. The interpretation must always be correlated with the patient's clinical presentation.
EEG Findings in Traumatic Brain Injury (TBI)
EEG changes following TBI vary depending on the severity and type of injury:
- Mild TBI (Concussion): EEG is often normal or may show transient, subtle changes like mild slowing or disorganization of the alpha rhythm, usually resolving quickly.
- Moderate to Severe TBI: More pronounced abnormalities are common. These can include:
- Diffuse Slowing: Increased theta and delta activity across the brain, reflecting generalized dysfunction, often related to the degree of brainstem involvement or diffuse axonal injury.
- Focal Slowing: Localized areas of slow-wave activity (theta/delta) often correspond to the site of a brain contusion or hematoma. The extent and severity of slowing can correlate with the size of the lesion.
- Suppression/Attenuation: Reduced amplitude of background rhythms, either focally over an injury site or more diffusely.
- Epileptiform Activity: Sharp waves, spikes, or spike-and-wave discharges may emerge, indicating an increased risk of post-traumatic seizures.
- Intracranial Hematomas:
- Epidural Hematoma: May initially show relatively localized slowing or suppression, sometimes with less prominent diffuse changes unless significant mass effect develops.
- Subdural Hematoma: Often associated with more significant diffuse changes (slowing, suppression) and potentially broader, less well-defined focal abnormalities or hemispheric asymmetry due to the widespread nature of the collection.
- Intracerebral Hematoma: Typically shows marked focal slowing (delta activity) overlying the hematoma, often accompanied by diffuse changes depending on the size and location.
In severe TBI with prolonged coma, EEG is crucial for monitoring brain function and assessing prognosis. Patterns range from diffuse slowing to more severe patterns like burst-suppression (periods of activity alternating with inactivity) or electrocerebral inactivity (flat line), indicating very poor prognosis or brain death. Certain patterns like "alpha coma" or "beta coma" (widespread alpha or beta activity in an unresponsive patient) also carry specific prognostic implications, often indicating severe brainstem or diffuse cortical injury.
Long-Term EEG Changes After TBI
In the chronic phase following TBI, EEG abnormalities may persist long after acute clinical symptoms resolve, especially after moderate to severe injuries. Persistent focal slowing or epileptiform discharges in the area of the original injury (contusion, hematoma site) are common findings and indicate areas of residual brain dysfunction and potential seizure focus development. Diffuse abnormalities may also persist due to ongoing issues with cerebral blood flow, CSF dynamics, or widespread neuronal damage.
References
- Niedermeyer E, Lopes da Silva F. Electroencephalography: Basic Principles, Clinical Applications, and Related Fields. 6th ed. Lippincott Williams & Wilkins; 2011. (Comprehensive textbook on EEG)
- Kane N, Acharya J, Benickzy S, et al. A practical guide to the routine EEG. Pract Neurol. 2017 Oct;17(5):397-407. DOI: 10.1136/practneurol-2017-001723. PMID: 28775131. (Guide to routine EEG practice)
- Tatum WO, Rubboli G, Kaplan PW, et al. Clinical utility of EEG in diagnosing and monitoring epilepsy in adults. Clin Neurophysiol. 2018 May;129(5):1056-1082. DOI: 10.1016/j.clinph.2018.02.128. PMID: 29604586. (Focuses on EEG utility in adult epilepsy)
- Vespa PM, Nuwer MR, Nenov V, et al. Increased incidence and impact of nonconvulsive and convulsive seizures after traumatic brain injury as detected by continuous electroencephalographic monitoring. J Neurosurg. 1999 Nov;91(5):750-60. DOI: 10.3171/jns.1999.91.5.0750. PMID: 10541230. (Study on EEG monitoring after TBI)
- Hirsch LJ, LaRoche SM, Gaspard N, et al. American Clinical Neurophysiology Society's Standardized Critical Care EEG Terminology: 2012 version. J Clin Neurophysiol. 2013 Feb;30(1):1-27. DOI: 10.1097/WNP.0b013e3182784729. PMID: 23377445. (Standardized terminology for critical care EEG)