Breaking down the skeleton’s structure
Checking out the skeleton’s makeup
This section is about how your body builds the tissues of the bones and the joints and how they all fit together to protect, move, and support the entire body.
Caring about connective tissue
The skeleton is made up mainly of three types of connective tissue: osseous (bone) tissue, cartilage, and fibrous connective tissue.
Osseous tissue
Osseous tissue is physiologically very active, constantly generating and repairing itself, and has a generous blood supply all through it. Not only that, but bone makes a huge amount of "product for export", notably the very cells of the blood. (Yes, new blood cells are made by bones — see Chapter 9.) Bone contains four specialized types of cells: osteocytes, osteoblasts, osteoclasts, and osteogenic cells. The skeletal system’s functions depend on the functioning of these specialized cells in bone tissue.
![]() Keep in mind the difference between bone tissue and a specific, named bone. Both the femur (thigh bone) and the humerus (arm bone) contain bone tissue, but each bone has its own specialized configuration of the components of bone tissue.
Keep in mind the difference between bone tissue and a specific, named bone. Both the femur (thigh bone) and the humerus (arm bone) contain bone tissue, but each bone has its own specialized configuration of the components of bone tissue.
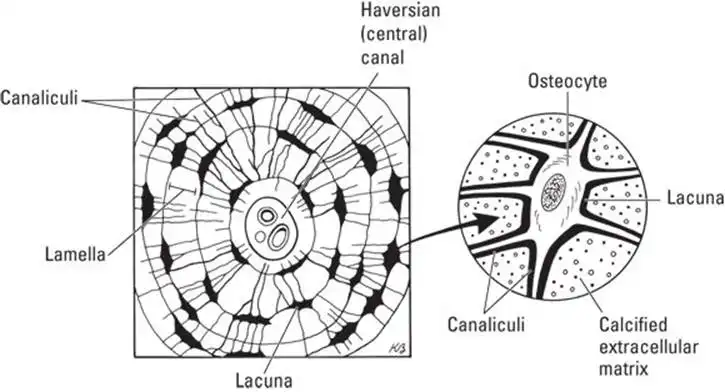
We think of our bones as being hard like rocks, and they are, but the structure of the osseous tissue is quite complex. Figure 5-1 shows the parts of osseous tissue.
The first thing you notice when looking at osseous tissue are the big holes. Then you see that everything seems to be arranged in circles around those holes. One set of these circles is called an osteon; these structures are repeated and glued together to form compact bone. The hole in the middle, the Haversian (or central) canal, creates space for the nerves and blood vessels to run throughout the bone.
Each ring encircling the central canal is called a lamella. These are formed as calcium compounds (such as calcium phosphate and calcium carbonate) are deposited into the matrix (the space between the cells). Unlike in other tissues where the matrix is fluid filled, bone cells, called osteocytes, are unable to move. They can be found in little caves called lacunae.
Also due to the rigid matrix, cells must get their nutrients from other cells. Osteocytes have armlike structures that reach through little tunnels through the matrix called canaliculi. Cells in the inner ring (lamella) have access to resources from the blood vessels in the central canal. They then pass these resources on to cells in the next ring through the canaliculi (tunnels). This continues, cell to cell, like a game of telephone.
Cartilage
Cartilage is a firm but flexible tissue made up of mostly protein fibers. If you put your finger on the end of your nose and push gently, you can get a very good idea of the rubbery texture and flexibility of cartilage. Cartilage is the main component of joints.
Cartilage is less complicated in its structure than bone tissue, having fewer cells, fewer cell types, and little or no direct blood supply. However, among the functions of cartilage tissue is the building of new bone. The two types of cartilage in the skeletal system are hyaline cartilage and fibrocartilage.
- Hyaline cartilage is the type that forms the septum of your nose. It also forms a portion of the very first version of the fetal skeleton. It’s the most abundant type of cartilage in several kinds of joints — it’s a major component of the freely movable ones called synovial joints.
- Fibrocartilage is a fibrous, spongy tissue that acts as a shock absorber in the vertebral column (spine) and the pelvis.
![]() Cartilage isn’t generated and replaced as actively as bone, so cartilage gets by with fewer cells, and mature cartilage has no blood supply.
Cartilage isn’t generated and replaced as actively as bone, so cartilage gets by with fewer cells, and mature cartilage has no blood supply.
![]() There is a third type of cartilage: elastic cartilage. Unlike the other two types, it contains numerous elastic fibers, making it much more flexible. You can find elastic cartilage in your epiglottis and your external ear.
There is a third type of cartilage: elastic cartilage. Unlike the other two types, it contains numerous elastic fibers, making it much more flexible. You can find elastic cartilage in your epiglottis and your external ear.
Fibrous connective tissue
Fibrous connective tissue (FCT) can be compared to the kind of packing tape that has fibers in it. FCT contains very few living cells and is composed mainly of protein fibers, complex sugars, and water.
FCT forms a structure called the periosteum, a protective sheet that covers bones. The collagen fibers in this covering intertwine with the collagen fibers of the tendons and ligaments. These cordlike structures connect a bone to another bone (ligaments), or a bone to a muscle (tendon).
![]() The periosteum is said to be continuous with the ligaments and tendon, because there’s no real separation between the "sheet" and the "cords." This prevents them from letting go of the bone.
The periosteum is said to be continuous with the ligaments and tendon, because there’s no real separation between the "sheet" and the "cords." This prevents them from letting go of the bone.
The structure of a bone
The structures called bones (the femur, the vertebrae, the finger bones) are made of bone tissue. (No surprise there, you say, but note that structures called joints are made of the tissue called cartilage.) It’s important to remember that different individual bones have different forms of bone tissue.
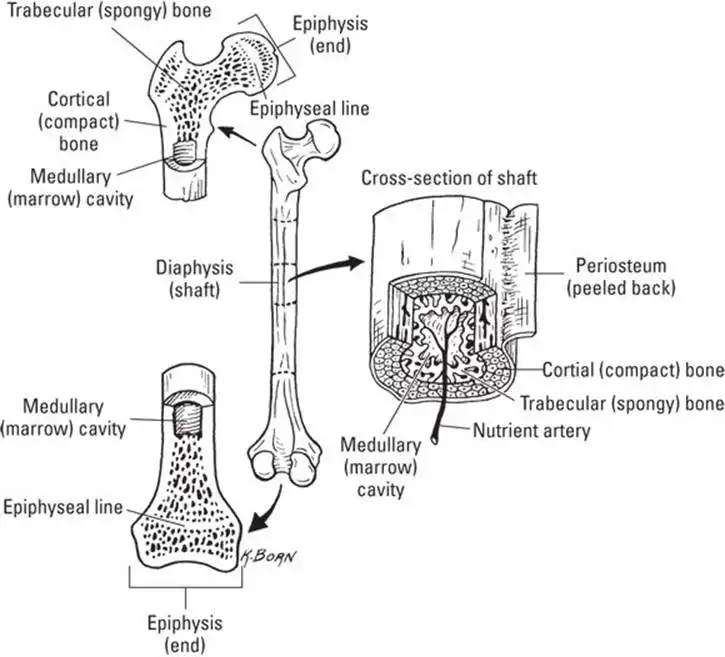
Long bones such as your thighbone (femur) or forearm bone (radius) are the type of bones people usually think of first. And in fact, they make a good illustration of general anatomy and physiology of bone tissue (see Figure 5-2).
In cross section, bone is structured in concentric layers, that is, an outer layer surrounds a middle layer, which in turn surrounds an inner layer. In longitudinal section, a bone has two ends, mostly similar, and a long middle area, which has cells and tissues mostly different from the ends. The following list names and briefly describes cellular and material composition of the areas of a long bone:
- Compact (cortical) bone (the outer layer) is a dense layer of cells in a hard matrix of protein fibers and compounds made of calcium and other minerals. This is the layer that gives bones their amazing strength. Compact bone tissue is described in detail in the "Caring about Connective Tissue" section, earlier in this chapter.
- Spongy (trabecular) bone (the middle layer) is, like compact bone, a variety of cell types within a matrix of mineralized protein fibers. But spongy bone has a more open structure than compact bone, a physiological trade-off between strength and lightness. The matrix of spongy bone is not arranged in concentric circles; instead, it appears, well, spongy. Structures called trabeculae, which follow stress lines in the bone, act like braces, providing support while leaving large pockets of space. In adults, this space contains red marrow, described in the next subsection.
- The medullary cavity is the inner layer of the shaft of a long bone (the diaphysis). The medullary cavity houses bone marrow, which comes in two varieties. There’s yellow marrow, which is mostly fat (think butter), and red marrow, the site of hematopoiesis, the production of blood cells. In adults, most of the marrow in the medullary cavity is deactivated and, thus, yellow. The active, red marrow is found in spongy bone of the skull, ribs, vertebrae, pelvis, and sternum (breastbone). In infants, medullary cavities of the long bones are mostly filled with red marrow to meet the increasing demand for blood cells.
- Epiphysis is the enlarged, knobby end of a long bone. It consists of an outer layer of compact bone overlying spongy bone. This is the site of bone elongation. Within the epiphysis, bone and cartilage tissue are intimately connected: As cartilage cells divide, cartilage morphs into bone tissue. This process continues from before birth until the bones reach their full adult size.
If blood cell levels drop too low — after blood loss, for instance — the yellow marrow can be reactivated and again perform hematopoiesis.
Classifying bones
Bones come in different shapes and sizes. Appropriately, many bone type names match what they look like, such as flat bones, long bones, short bones, and irregular bones. Check out Table 5-1 for the differences among the four types of bones.
TABLE 5-1 Characteristics of Bone Types
| Bone Type | Example Location in the Body | Characteristics |
| Flat | Skull, shoulder blades, ribs, sternum, pelvic bones | Like plates of armor, flat bones protect soft tissues of the brain and organs in the thorax and pelvis. |
| Long | Arms and legs | Like steel beams, these weight-bearing bones provide structural support. |
| Short | Wrists (carpal bones) and ankles (tarsal bones) | Short bones look like blocks and allow a wider range of movement than larger bones. |
| Irregular | Vertebral column, kneecaps | Irregular bones have a variety of shapes and usually have projections that muscles, tendons, and ligaments can attach to. |
Bone growth and remodeling
When long bones develop in a fetus, they’re formed from hyaline cartilage. The softer cartilage allows the fetus to bend into the poses that would make a yoga instructor beam with pride. The shape of the bone is determined by the shape of the cartilage, so it serves as a template. Calcium compounds are deposited onto the template, and the cartilage becomes calcified.
![]() The terms calcification and ossification are often used synonymously to refer to the formation of bone. However, ossification is properly the formation of the whole tissue, whereas calcification is the actual formation and deposition of the calcium compounds.
The terms calcification and ossification are often used synonymously to refer to the formation of bone. However, ossification is properly the formation of the whole tissue, whereas calcification is the actual formation and deposition of the calcium compounds.
Even at birth, the bones are not fully ossified. They continue to grow and develop well into the teenage years. This occurs via two types of ossification:
- Intramembranous ossification: Intramembranous ossification occurs in all bones; it’s how short, flat, and irregular bones grow in size, and it’s how long bones increase their width. A sheet of connective tissue is formed beneath the periosteum. Specialized bone cells called osteoblasts place the calcium compounds onto the fibers of the connective tissue, creating the trabeculae of spongy bone (calcification). When they’re done building, osteoblasts become osteocytes. Later, the new spongy bone can be further developed into compact bone as new osteoblasts fill the empty space with calcium compounds until they’ve walled themselves in to a little cave — a lacuna.
- Endochondral ossification: To increase their length, long bones use endochondral ossification. In Figure 5-2, you see an epiphyseal line on each end. Rather than being osseous tissue, the epiphyseal line (or plate) is made of hyaline cartilage. When stimulated by growth hormone (see Chapter 8), the chondrocytes (cartilage cells) begin to copy themselves. The cells will then enlarge, which creates more space, thus lengthening the bone. Osteoblasts will then calcify the cartilage just as they did to the connective tissue during intramembranous growth.
When the long bones increase in length, you increase in height. Eventually, around age 18, the chondrocytes stop dividing. The entire epiphyseal line is ossified (turned into bone). This is commonly referred to as the growth plates being closed.
While you’re likely done growing at this point in your life, your bones are definitely not done developing. This continues throughout life via a process called remodeling.
Because bones are constantly absorbing the forces placed on our bodies, the matrix gets damaged. The remodeling process allows the bones to retain their structural integrity by constantly replacing the weakened tissue with strong, healthy matrix. It works like road construction. The roads wear out with continued use and need to be refreshed. But you can’t do all the roads at once or else people wouldn’t be able to get places. So you do it in sections at a time, all the time. Luckily, bone remodeling doesn’t cause the headaches that road construction does!
Before we can activate osteoblasts to build new tissue, we must first clear the area. Specialized bone cells called osteoclasts are responsible for this task. Osteoclasts secrete acid to break down the weakened matrix. This releases the calcium ions from their compounds, allowing them to be absorbed into blood flow. Then osteoblasts recycle the calcium, building new compounds to deposit and reform the matrix stronger than before.
![]() The forgotten function of bones is to store calcium, an ion essential for both muscle contraction and nervous communication (see Chapters 6 and Chapters 7). When blood calcium levels drop too low, parathyroid hormone (PTH) is released and proceeds to the bones. The PTH then stimulates osteoclasts to resorb the calcium.
The forgotten function of bones is to store calcium, an ion essential for both muscle contraction and nervous communication (see Chapters 6 and Chapters 7). When blood calcium levels drop too low, parathyroid hormone (PTH) is released and proceeds to the bones. The PTH then stimulates osteoclasts to resorb the calcium.
See also
- Locating Physiology on the Web of Knowledge
- Chapter 1. Anatomy and Physiology: The Big Picture
- Chapter 2. What Your Body Does All Day
- Chapter 3. A Bit about Cell Biology
- Sizing Up the Structural Layers
- Chapter 4. Getting the Skinny on Skin, Hair, and Nails
- Chapter 5. Scrutinizing the Skeletal System
- Chapter 6. Muscles: Setting You in Motion
- Talking to Yourself
- Chapter 7. The Nervous System: Your Body’s Circuit Board
- Chapter 8. The Endocrine System: Releasing Chemical Messages
- Exploring the Inner Workings of the Body
- Chapter 9. The Cardiovascular System: Getting Your Blood Pumping
- Chapter 10. The Respiratory System: Breathing Life into Your Body
- Chapter 11. The Digestive System: Beginning the Breakdown
- Chapter 12. The Urinary System: Cleaning Up the Act
- Chapter 13. The Lymphatic System: Living in a Microbe Jungle
- Life’s Rich Pageant: Reproduction and Development
- Chapter 14. The Reproductive System
- Chapter 15. Change and Development over the Life Span
- The Part of Tens
- Chapter 16. Ten (Or So) Chemistry Concepts Related to Anatomy and Physiology
- Chapter 17. Ten Phabulous Physiology Phacts
- Supplemental Images