Upper Respiratory Infection (URTI)
- What Is It?
- Contagious
- Causes
- Symptoms
- Risk and Complications
- Diagnosis
- Treatment
- Home Remedies
- Alternative Therapies
- Prevention

Upper respiratory tract infection (URTI) definition and facts
- Upper respiratory infections (URIs) are one of the most common reasons for doctor visits.
- Upper respiratory infections are the most common illness resulting in missed work or school.
- Upper respiratory tract infections can happen at any time but are most common in the fall and winter.
- The vast majority of upper respiratory infections are caused by viruses and are self-limited.
- Symptoms of upper respiratory infection include
- cough,
- sneezing,
- nasal discharge,
- nasal congestion,
- runny nose,
- fever,
- scratchy or sore throat, and
- nasal breathing.
- Antibiotics are rarely needed to treat upper respiratory infections and generally should be avoided unless the doctor suspects a bacterial infection.
- Simple techniques, such as proper handwashing and covering the face while coughing or sneezing, may reduce the spread of respiratory tract infections.
- The general outlook for upper respiratory infections is favorable, although, sometimes complications can occur.
What is an upper respiratory infection?
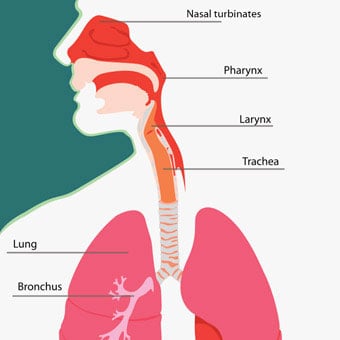
The upper respiratory tract includes the sinuses, nasal passages, pharynx, and larynx. These structures direct the air we breathe from the outside to the trachea and eventually to the lungs for respiration to take place.
An upper respiratory tract infection, or upper respiratory infection, is an infectious process of any of the components of the upper airway.
Infection of the specific areas of the upper respiratory tract can be named specifically. Examples of these may include rhinitis (inflammation of the nasal cavity), sinus infection (sinusitis or rhinosinusitis) -- inflammation of the sinuses located around the nose, common cold (nasopharyngitis) -- inflammation of the nares, pharynx, hypopharynx, uvula, and tonsils, pharyngitis (inflammation of the pharynx, uvula, and tonsils), epiglottitis (inflammation of the upper portion of the larynx or the epiglottis), laryngitis (inflammation of the larynx), laryngotracheitis (inflammation of the larynx and the trachea), and tracheitis (inflammation of the trachea).
Upper respiratory infections are one of the most frequent causes for a doctor visit with varying symptoms ranging from a runny nose, sore throat, cough, to breathing difficulty, and lethargy. In the United States, upper respiratory infections are the most common illness leading to missing school or work.
Although upper respiratory infections can happen at any time, they are most common in the fall and winter months, from September until March. This may be explained because these are the usual school months when children and adolescents spend a lot of time in groups and inside closed doors. Furthermore, many viruses of upper respiratory infection thrive in the low humidity of the winter.

Is an upper respiratory infection contagious?
A majority of upper respiratory infections are due to self-limited viral infections. Occasionally, bacterial infections may cause upper respiratory infections. Most often, upper respiratory infection is contagious and can spread from person to person by inhaling respiratory droplets from coughing or sneezing. The transmission of respiratory infections can also occur by touching the nose or mouth by hand or other objects exposed to the virus.

What are the causes of upper respiratory infection?
The URTI is generally caused by the direct invasion of the inner lining (mucosa or mucus membrane) of the upper airway by the culprit virus or bacteria. In order for the pathogens (viruses and bacteria) to invade the mucus membrane of the upper airways, they have to fight through several physical and immunologic barriers.
The hair in the lining of the nose acts as a physical barrier and can potentially trap the invading organisms. Additionally, the wet mucus inside the nasal cavity can engulf the viruses and bacteria that enter the upper airways. There are also small hair-like structures (cilia) that line the trachea which constantly moves any foreign invaders up towards the pharynx to be eventually swallowed into the digestive tract and into the stomach.
In addition to these intense physical barriers in the upper respiratory tract, the immune system also does its part to fight the invasion of the pathogens or microbes entering the upper airway. Adenoids and tonsils located in the upper respiratory tract are a part of the immune system that helps fight infections. Through the actions of the specialized cells, antibodies, and chemicals within these lymph nodes, invading microbes are engulfed within them and are eventually destroyed.
Despite these defense processes, invading viruses and bacteria adopt various mechanisms to resist destruction. They can sometimes produce toxins to impair the body's defense system or change their shape or outer structural proteins to disguise from being recognized by the immune systems (change of antigenicity). Some bacteria may produce adhesion factors that allow them to stick to the mucus membrane and hinder their destruction.
It is also important to note that different pathogens have varying abilities to overcome the body's defense system and cause infections.
Furthermore, different organisms require a varying time of onset from when they enter the body to when symptoms occur (incubation time). Some of the common pathogens for upper respiratory infection and their respective incubation times are the following:
The table shows the incubation period of the common pathogens for an upper respiratory infection.
| Virus and Bacteria Organisms | Incubation time (Days) |
|---|---|
| Rhinoviruses | 1 - 5 |
| Group A streptococci | 1 - 5 |
| Influenza and parainfluenza viruses | 1 - 4 |
| Respiratory syncytial virus (RSV) | 7 |
| Whooping cough (pertussis) | 7 - 21 |
| Diphtheria | 1 - 10 |
| Epstein-Barr virus (EBV) | 4 - 6 weeks |

What are the symptoms of upper respiratory infection?
Generally, the symptoms of upper respiratory infection result from the toxins released by the pathogens as well as the inflammatory response mounted by the immune system to fight the infection.
Common symptoms of upper respiratory infection generally include:
- nasal congestion,
- runny nose (rhinorrhea),
- nasal discharge (may change from clear to white to green)
- nasal breathing,
- sneezing,
- sore or scratchy throat,
- painful swallowing (odynophagia),
- cough (from laryngeal swelling and post nasal drip),
- malaise, and
- low-grade fever (more common in children).
Other less common symptoms may include
- foul breath,
- reduced ability to smell (hyposmia),
- headache,
- shortness of breath,
- sinus pain,
- itchy and watery eye (conjunctivitis),
- nausea,
- vomiting
- diarrhea, and
- body aches.
The symptoms of upper respiratory infection usually last between 3-14 days; if symptoms last longer than 14 days, an alternative diagnosis can be considered such as:
Bacterial pharyngitis (strep throat due to group A Streptococcus) may be considered if symptoms continue to worsen after the first week in the absence of runny nose, cough, or conjunctivitis. Prompt testing and initiation of appropriate antibiotics is important due to the risk of developing rheumatic fever, especially in children.
Epiglottitis is an upper respiratory infection in children that may have a more sudden onset of sore throat, feeling of a lump in the throat, muffled voice, dry cough, very painful swallowing, and drooling.
Respiratory infections in the lower part of the upper respiratory tract, such as, laryngotracheitis, are more commonly featured with dry cough and hoarseness or loss of voice. Barking or whooping cough, gagging, rib pain (from severe cough) are other symptoms and signs.

What are the risk factors for upper respiratory infection?
Some common risk factors for upper respiratory infection are:
- physical or close contact with someone with an upper respiratory infection;
- poor hand washing after contact with an individual with upper respiratory infection;
- close contact with children in a group setting, schools, or daycare centers;
- contact with groups of individuals in a closed setting, such as traveling, tours, cruises;
- smoking or second-hand smoking (may impair mucosal resistance and destroy the cilia);
- health care facilities, hospitals, nursing homes;
- immunocompromised state (compromised immune system) such as HIV, organ transplant, congenital immune defects, long term steroid use; and
- anatomical abnormalities as in facial trauma, upper airway trauma, nasal polyps.
When should you seek medical care for a respiratory tract infection?
Most people tend to diagnose and treat their symptoms at home without seeking professional medical care. A great majority of cases of upper respiratory infection are caused by viruses and are self-limited, meaning they resolve on their own spontaneously.
Visiting a doctor may be advisable if:
- symptoms last more than a couple of weeks,
- symptoms are severe and worsening,
- there is difficulty breathing,
- swallowing is impaired, and
- upper respiratory infection is recurring.
Sometimes hospitalization may be necessary if the upper respiratory infection is severe and causes significant dehydration, respiratory difficulty with poor oxygenation (hypoxia), significant confusion, lethargy, and worsening of shortness of breath in chronic lung and heart disease (chronic obstructive pulmonary disease or COPD, congestive heart failure). Hospitalizations are much more common in children less than 2 years of age, elderly people (especially those with dementia), and immunocompromised individuals (weak immune system).

How is an upper respiratory infection diagnosed?
In evaluating people with a suspected upper respiratory infection, other alternative diagnoses need to be considered. Some of the common and important diagnoses that can resemble upper respiratory infection are:
- asthma,
- pneumonia,
- H1N1 (swine) flu,
- influenza,
- allergic reactions,
- seasonal allergies,
- chronic (long-standing) sinusitis,
- acute HIV infection, and
- bronchitis.
The diagnosis of upper respiratory infection is typically made based on a review of symptoms, physical examination, and occasionally, laboratory tests.
In a physical examination of an individual with an upper respiratory infection, a doctor may look for swollen and redness inside the wall of the nasal cavity (a sign of inflammation), redness of the throat, enlargement of the tonsils, white secretions on the tonsils (exudates), enlarged lymph nodes around the head and neck, redness of the eyes, and facial tenderness (sinusitis). Other signs may include bad breath (halitosis), cough, voice hoarseness, and fever.
Laboratory testing is generally not recommended in the evaluation of upper respiratory infections. Because most upper respiratory infections are caused by viruses, specific testing is not required as there is typically no specific treatment for different types of viral upper respiratory infections.
Some important situations where specific testing may be important include:
- Suspected strep throat (fever, lymph nodes in the neck, whitish tonsils, absence of cough), necessitating rapid antigen testing (rapid strep test) to rule in or rule out the condition given possible severe sequelae if untreated.
- Possible bacterial infection by taking bacterial cultures with a nasal swab, throat swab, or sputum.
- Prolonged symptoms, as finding a specific virus can prevent unnecessary use of antibiotics (for example, rapid testing for the influenza virus from nasal or pharyngeal swabs).
- Evaluation of allergies and asthma which can cause long-lasting or unusual symptoms.
- Enlarged lymph node and sore throat as the primary symptoms that may be caused by the Ebstein-Barr virus (mononucleosis) with an expected longer time course (by using the monospot test).
- Testing for the H1N1 (swine) flu is suspected.
Blood work and imaging tests are rarely necessary for the valuation of upper respiratory infection. X-rays of the neck may be done if a suspected case of epiglottitis. Although the finding of swollen epiglottis may not be diagnostic, its absence can rule out the condition. CT scans can sometimes be useful if symptoms suggestive of sinusitis last longer than 4 weeks or are associated with visual changes, copious nasal discharge, or protrusion of the eye. CT scan can determine the extent of sinus inflammation, the formation of an abscess, or the spread of infection into adjacent structures (cavity of the eye or the brain).

What is the treatment for upper respiratory infection?
As described above, most cases of upper respiratory infection are caused by viruses and therefore, require no specific treatment and are self-limited. People with upper respiratory infections typically diagnose themselves and treat their symptoms at home without requiring a doctor's visit or prescription medications.
Rest is an important step in treating upper respiratory infections. Usual activities, such as working and light exercising may be continued as much as tolerated.
Increased intake of oral fluids is also generally advised to keep up with the fluid loss from a runny nose, fevers, and poor appetite associated with upper respiratory infections.
Treatment of the symptoms of upper respiratory infection is usually continued until the infection has resolved.
Some of the most common upper respiratory infection or cold medications used to treat these symptoms are the following:
- Acetaminophen (Tylenol) can be used to reduce fever and body aches.
- Nonsteroidal anti-inflammatory drugs such as ibuprofen (Motrin, Advil) can be used for body aches and fever.
- Antihistamines such as diphenhydramine (Benadryl) are helpful in decreasing nasal secretions and congestions.
- Nasal ipratropium (topical) can be used to diminish nasal secretions.
- Cough medications (antitussives) can be used to reduce cough. Many cough medications are commercially available such as dextromethorphan, guaifenesin (Robitussin), and codeine all have shown benefits in reducing cough in upper respiratory infections.
- Honey can be used in reducing cough.
- Steroids such as dexamethasone (Decadron) and prednisone orally (and nasally) are sometimes used to reduce inflammation of the airway passage and decrease swelling and congestion.
- Decongestants such as pseudoephedrine (Sudafed) Actifed oral, phenylephrine (Neo-synephrine nasal) can be used to reduce nasal congestion (generally not recommended in children less than 2 years of age and not recommended for individuals with high blood pressure).
- Oxymetazoline (Afrin) nasal solution is a decongestant, but should only be used for short-term.
- Combination medications containing many of these components are also widely available over the counter.
Some cough and cold medicines that can cause excessive drowsiness need to be used with caution in children younger than 4 years of age and the elderly.
Broad-spectrum antibiotics are sometimes used to treat upper respiratory infections if a bacterial infection is suspected or diagnosed. These conditions may include strep throat, bacterial sinusitis, or epiglottitis. Antivirals may occasionally be recommended by doctors in patients who are immunocompromised (poor immune system). The treating doctor can determine which antibiotic would be the best option for a particular infection.
Because antibiotic use is associated with many side effects and can promote bacterial resistance and secondary infections, they need to be used very cautiously and only under the direction of a treating physician.
Inhaled epinephrine is sometimes used in children with severe spasms of the airways (bronchospasm) and in croup to reduce spam.
Rarely, surgical procedures may be necessary in cases of complicated sinus infections, compromised airway with difficulty breathing, the formation of abscesses behind the throat, or abscess formation of the tonsils (peritonsillar abscess).

What are home remedies for upper respiratory infection?
Several self-care methods can simply be applied at home for relief of symptoms of upper respiratory infection.
Moist warm air can help soothe the oral and nasal passages that become more irritated with dry air. This can make breathing easier and nasal secretions looser and easier to discharge. Some simple ways to do this are:
- making steam in the shower by turning on the hot water (without going under it) and breathing the steamed air;
- drinking warm beverages (hot tea, hot chocolate, warm milk);
- using a vaporizer to create humidity in the room; and
- avoid cold, dry air if possible.
Nasal saline (saltwater) can help with symptoms of nasal congestion. There are over-the-counter saline spray solutions available that can be used for this purpose. Simpler and more cost-effective home-made saltwater solution may also be considered. A fourth of a teaspoon of salt can be added to an 8 oz cup of room temperature water and stirred to dissolve. Using a bulb syringe or a small spray bottle, the solution may be applied in one nostril at a time with slow inhalation and expelled with exhalation several times a day as needed.
Applying a warm pack (a warm well towel or washcloth) to the face may also be used to treat symptoms of nasal congestion. This can be repeated every few hours as needed to relieve the symptoms.
Saltwater gurgles and lozenges may reduce throat irritation and dryness and can alleviate the symptoms of throat symptoms.
Cough can be suppressed by limiting exposure to irritants, such as cold weather, cigarette smoke, dust, and pollution. Sleeping in a semi-upright position may be helpful at times to reduce cough. A study has suggested that honey may be superior to dextromethorphan in reducing cough in children with an upper respiratory infection.
Adequate hydration with water, juices, and non-caffeinated drinks can thin nasal secretions and replace the fluid losses.

What are some data on alternative therapies in treating upper respiratory infections?
Many alternative and cultural remedies are used in treating upper respiratory infections.
Herbal teas including elm bark and licorice root are thought to relieve sore throat and some studies have suggested benefits compared to placebo. Long-term use of these remedies has not been evaluated; however, prolonged use of licorice may cause elevation of blood pressure.
As noted above, honey has been shown to be beneficial in suppressing cough in children with an upper respiratory infection and its use in hot water or tea with lemon juice is not uncommon. Ingestion of honey in infants, however, is not recommended as they are not able to properly digest the spores in honey which can result in infections.
Echinacea is another herbal remedy commonly used in treating upper respiratory infection. Research data failed to prove any significant benefit in altering the duration and severity of upper respiratory infection symptoms when Echinacea was used in children between 2-11 years of age as compared to placebo.
Oral zinc supplementation has been used in recent years to shorten the duration and reduce the severity of symptoms of upper respiratory infection and the common cold. This therapy has been studied in children with an upper respiratory infection and the results are mixed. The FDA has not approved the use of oral zinc to treat the common cold or upper respiratory infections. There are reports of nausea and unpleasant taste caused by oral zinc.
Topical nasal zinc products (Zicam nasal gel) have been also used to attenuate the symptoms of upper respiratory infection. Some studies suggest the loss of the sense of smell (anosmia) associated with the use of this over-the-counter product. Therefore, the FDA recommended discontinuation of the use of intranasal zinc products in 2009.
The use of oral vitamin C is thought to shorten the duration of upper respiratory infection symptoms, but research data are inconclusive regarding the benefits of vitamin C.
What are the complications of an upper respiratory infection?
Some of the common complications of upper respiratory infections are the following:
- respiratory compromise from epiglottitis;
- secondary infection by bacteria (viral infection can cause impairment of the physical barrier in the respiratory airways making it easier for bacteria to invade) resulting in bacterial sinusitis, bronchitis, pneumonia;
- formation of abscesses in the tonsils;
- rheumatic fever from strep throat;
- spread of infection from sinuses to the brain (meningitis);
- involvement of the ears resulting in middle ear infections (otitis media);
- worsening of underlying chronic lung disease (asthma, COPD);
- spread of infection to the heart (pericarditis, myocarditis);
- spread of the infection to the brain or the fluid around the brain causing encephalitis or meningitis; and
- muscular pain and rib fractures from forceful coughing.

Can an upper respiratory infection be prevented?
There are several measures that can reduce the risk of infections in general. Smoking cessation, reducing stress, and adequate and balanced diet, and regular exercise are all measures that can improve the immune system and reduce the overall risk of infections. Breastfeeding also helps strengthen the immune system of infants by transferring the protective antibodies from the mother's milk to the baby.
Other preventive measures to diminish the risk of spread of upper respiratory infections are:
- a hand washing is especially encouraged during the cold seasons (fall and winter) or handling others with the infection;
- reducing contact with people who may have the infection (people may carry and spread the virus a few days before they have symptoms and a few days after their symptoms have resolved);
- proper cleaning of common objects that are touched by individuals who may be infectious such as, telephones, refrigerator door, computers, stair railings, door handles, etc.;
- covering mouth and nose when coughing or sneezing; and
- vaccination with flu vaccine as recommended for certain people (elderly, people with chronic medical conditions, health care workers, etc.).

What is the outlook for a patient suffering from an upper respiratory infection?
In general, the outcome of upper respiratory infection is good. The majority of these cases are due to viral infections that are self-limiting. Bacterial infections, people with weak immune systems, and those with complications of upper respiratory infections (listed above) may have a less favorable prognosis.


