Streptococcal Infections
- Facts
- Causes
- Are They Contagious?
- Contagious Period
- Incubation Period
- Signs/Symptoms
- Invasive GAS disease
- Necrotizing Fascitis
- Toxic Shock Syndrome
- Diagnosis
- Treatment
- Specialists
- Complications
- Prevention
- Prognosis
- More Info
Group A streptococcal infections (GAS) facts
- Group A streptococci (GAS) are defined gram-positive spherical-shaped bacteria that produce beta-hemolysis (lysis of red blood cells producing clear or transparent areas in special growth media) and appear usually as a chain of two or more bacteria and have molecules on their surface known as Lancefield group A antigens.
- Group A Streptococcus (GAS) organisms are usually spread by direct human-to-human transfer. Occasionally, they can be spread by droplets or by a person touching items recently handled by an infected individual (also termed fomites).
- GAS can cause a wide range of diseases, but most notably streptococcal pharyngitis (strep throat) in school-aged children and teens; other diseases (or complications) include fever, rheumatic fever, kidney damage, wound and skin infections (for example, impetigo), and occasionally, necrotizing fasciitis and shock.
- Some GAS infections are contagious, and others are not.
- GAS infections that are contagious can be contagious during the incubation period (the time between infection and development of symptoms) until symptoms stop.
- The incubation period varies according to the specific GAS-caused infection, but most have a range of about one to five days while others take over a week to cause symptoms.
- Symptoms and signs of GAS disease are variable and are related to the body area that is affected by the infection; for example, sore throat, throat erythema, and swollen lymph nodes in strep throat to low blood pressure and organ failure in streptococcal toxic shock syndrome (STSS).
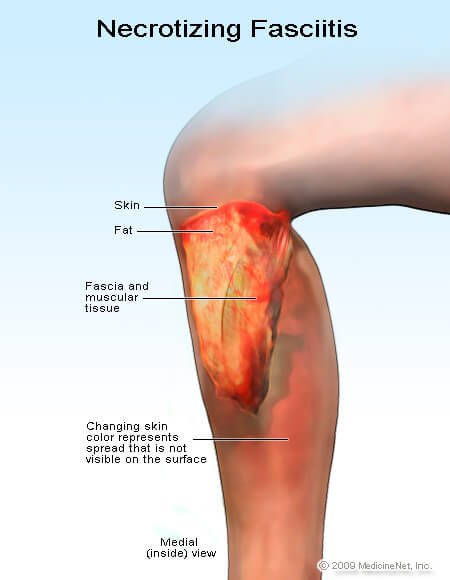
- Early signs and symptoms of necrotizing fasciitis include fever, severe pain and swelling, and erythema (redness) at the wound site or site where GAS organisms entered the body; later signs and symptoms include fluid discharge from the infected tissue, skin loss, and low blood pressure
- Early symptoms of toxic shock syndrome are nonspecific, often begin with flu-like symptoms of mild fever and malaise, then the condition often suddenly advances with symptoms of high fever, nausea, vomiting, diarrhea, skin rash, and low blood pressure with possible progression to include confusion, headaches, seizures, and skin loss from the palms of the hands and from the soles of the feet.
- Diagnosis of GAS is made by culturing the bacteria and having the laboratory identify the bacteria by metabolic functions and immunologic tests; rapid tests are based on immunological recognition of GAS antigens taken from the patient by swabbing the throat.
- Although oral antibiotics (many types) are effective in treating milder forms of GAS infections, more serious forms of GAS such as invasive GAS disease usually require multiple antibiotics administered IV; in addition, some patients may require surgery to remove dead and dying tissue.
- Infectious-disease specialists, pediatricians, OB/GYN specialists, critical care specialists, dermatologists, internal-medicine specialists, family practitioners, and surgeons may be involved in the team caring for a GAS patient.
- The prognosis (outcome) of GAS infections, especially mild infections, is usually good to excellent. However, as the disease progresses from moderate to life-threatening, the prognosis decreases from good to poor; early effective treatment may improve the prognosis.
- Prevention of GAS infections is possible by attention to good hygiene such as hand washing and avoiding eating or drinking from the same containers used by other people and avoiding direct and indirect (for example, droplet or particle contamination of clothing) contact with an infected individual; early treatment of GAS infections can reduce or prevent the progression to more severe disease.
- Although research is ongoing, there is no commercially available vaccine to prevent GAS infections.
What is group A Streptococcus (GAS)?

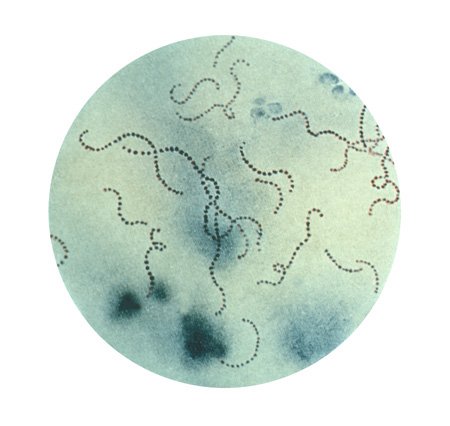
Group A Streptococcus is defined as a gram-positive bacterial genus composed of Streptococcus pyogenes strains. Group A Streptococcus strains have a similar surface antigen recognized by specific laboratory tests, termed the Lancefield group A antigen. Lancefield groups (about 18 Lancefield groups) are composed of different Streptococcus species groups with specific antigens and are distinguished by specific antibody tests. Besides, group A Streptococcus strains are beta-hemolytic (beta-hemolytic means the bacteria lyse red blood cells suspended in agar plates with secreted substances, see, for example, Fig. 3). These tests are mentioned because they are frequently used to distinguish group A Streptococcus bacteria from group B, group C, and other Streptococcus groups. Group A Streptococcus bacteria appear as pairs and chains when gram-stained (see Fig. 1); these bacteria are also termed "beta strep, GAS, and GABHS." Although these bacteria can harmlessly colonize people on their throats and skin, sometimes they can cause mild to serious diseases. GAS bacteria have been causing diseases in humans probably since humans first developed.
Streptococcus pyogenes (GAS) bacteria have many components that contribute to the pathogen's ability to cause disease:
- Lipoteichoic acid on its surface helps the GAS bacteria to bind to epithelial cell membranes.
- M proteins (over 100 types on the GAS bacterial strains) help the bacteria resist immunologic host defenses.
- Exotoxins (for example, DNAses A, C and D, streptolysin S, proteinase, streptokinase, and pyrogenic exotoxins [A-D])
- Human immune system stimulators (for example, streptolysin O, DNAse B, and hyaluronidase)
Exotoxins cause scarlet fever rash, damage organs, may cause shock, and inhibit the human immune system, while the human immune system stimulators may stimulate the immune system to produce antibodies that likely play a role in the development of autoimmune responses that can lead to glomerulonephritis or acute rheumatic fever. S. pyogenes (GAS) has over 100 serotypes that may vary somewhat in their ability to produce the above components that contribute to the pathogenicity of each strain of bacteria. In 2015, a new GAS strain, known as genotype emm89, was noted in the United Kingdom; the genetic changes seemed to enhance the strain's ability to cause disease and seems to be replacing older GAS genotypes.
How do people contract group A streptococcal (GAS) infections?
In most instances, GAS bacteria are contracted via person-to-person contact with mucus, skin, or infected lesions. Spread of the GAS organisms occurs infrequently by items that have made contact with infected people. However, many people are colonized (have the bacteria on body surfaces but are not infected) with GAS bacteria. Infants and children often first acquire these organisms from their colonized mothers.
What diseases are caused by group A streptococcal infection?
There are a number of diseases that GAS organisms can cause. The predominant diseases are as follows:
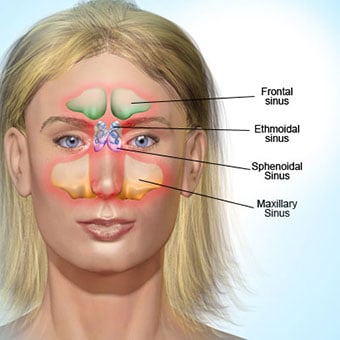
- Streptococcal pharyngitis (strep throat, Fig. 2)
- Scarlet fever
- Rheumatic fever
- Glomerulonephritis
- Impetigo
- Cellulitis (almost anywhere on the body; see erysipelas below)
- Wound infections
- Bone infections
- Sinusitis
- Pneumonia
- Meningitis
- Necrotizing fasciitis (sometimes termed a flesh-eating disease)
- Streptococcal toxic shock syndrome
- Tonsillopharyngitis
- Puerperal fever (fever after pregnant female delivers)
- Erysipelas (cellulitis of the skin, often the facial skin)
This list is not exhaustive as GAS bacteria have been found in many other disease processes. In addition, many of the diseases listed above may also be caused by many other pathogens, although the first three listed (pharyngitis, scarlet fever, and rheumatic fever) are predominantly caused by GAS. Some investigators consider most of these diseases as complications of an initial GAS skin or throat infection.
Are group A strep infections contagious?
In general, group A strep infections are contagious, but there are some qualifiers to this answer. For example, strep throat is contagious, but other infection types such as toxic shock syndrome are generally considered noncontagious; consequently, the answer depends on the specific type of infection and any extenuating circumstances.
What is the contagious period for group A strep infections?
For those infections that are considered to be contagious, the person is contagious in the incubation period (before any symptoms of the infection develop) and through the acute phase of the infection while the patient has symptoms. When symptoms stop, the person is usually noncontagious unless the individual becomes a carrier (colonized with group A strep but without symptoms).
What is the incubation period for group A strep infections?
The incubation period for GAS pharyngitis and cellulitis varies from about one to five days. Other types of GAS infection may develop rapidly (necrotizing fasciitis) while others (scarlet fever) may take a week or more to develop.
What are the signs and symptoms of group A strep infections?
GAS infections can produce many different signs and symptoms:
- Pharyngitis (strep throat/tonsillitis): sore throat, irritation with swallowing, white patches on tonsils (exudates), swollen lymph nodes on the neck, fever; pharyngitis with fever and white patches on tonsils are important but not definitive signs of GAS pharyngitis.
- Scarlet fever: pharyngitis symptoms (see above), pastia (pink or red lines formed of confluent petechiae, which are small purple or red spots in the skin caused by minor blood vessel breaks) that are found in skin creases, especially the flexor surface of the elbow), fever, rash on neck and chest, then entire body with sandpaper texture, muscle aches, abdominal pain, swollen red tongue (strawberry tongue)
- Rheumatic fever: inflammation of the joints, heart valve damage
- Glomerulonephritis: inflammation of the kidneys, impaired kidney function
- Necrotizing fasciitis: tissue destruction that progresses rapidly
- Toxic shock syndrome: rapidly progressing organ failure with low blood pressure
Most of the diseases listed here for GAS infection usually occur after an initial pharyngitis, with necrotizing fasciitis and toxic shock sometimes occurring without a detectable initial pharyngitis infection. Other disease processes involving GAS organisms (for example, meningitis, bone infections, pneumonia, wound infections, and others) produce the typical symptoms associated with these disease processes and clinically are not unique for GAS or other pathogenic organisms.
What is invasive group A streptococcal disease? Who is most at risk for getting invasive GAS disease?
Invasive GAS disease is when GAS organisms invade and infect organs or organ systems in the body (for example, GAS infections of the blood, muscle, fatty tissue, or the lungs). These are serious infections, and the mortality rate (death rate) varies from about 10%-60%, depending on the area(s) of the body infected. The most severe forms of invasive GAS infections are with necrotizing fasciitis and streptococcal toxic shock syndrome described below. People at higher risk for getting invasive forms of GAS are individuals with chronic diseases and immunosuppressed patients (for example, cancer, diabetes, and renal failure patients, and people taking steroid-type medications). Most healthy people do not get this type of GAS disease, but if they have skin breaks (cuts, abrasions, recent surgical sites), these individuals have a higher risk of GAS disease than people without skin breaks.
Other patients who are at risk for invasive GAS disease are patients with GAS infections that can easily progress into deep fat and muscle (for example, a GAS infection near the scrotum or anus or an abscess in the skin) and can progress to necrotizing fasciitis. Toxic shock syndrome was initially found to be associated with vaginal infections secondary to tampon use (or inappropriate use such as leaving a tampon in the vagina for an extended time). However, any patient who has a wound or surgery that requires packing to reduce bleeding (for example, nasal packing for severe nose bleeding) is at increased risk for toxic shock syndrome. Toxic shock syndrome may also be caused by a different bacterium called Staphylococcus.
Consequently, risk factors for GAS organisms to cause infection include suppression of the immune system (see above), open wounds or wound packing, or tampons that may promote GAS survival and proliferation. Children and the elderly are at higher risk to become infected with GAS.
What are the symptoms and signs of necrotizing fasciitis?
Early signs and symptoms of necrotizing fasciitis include fever, severe pain, swelling, and erythema (redness) at the wound site or site where GAS organisms entered the body. The pain and swelling may extend well beyond the erythema. Skin changes may resemble cellulitis initially, but ulceration, scabs, and fluid draining from the site develop, sometimes rapidly (Fig. 3). GAS organisms then can spread to the bloodstream and the patient can develop bacteremia and septic shock with high fever and a low blood pressure. About 20% of patients with necrotizing fasciitis caused by GAS will die from the infection.
What are the signs and symptoms of streptococcal toxic shock syndrome (STSS)?
Early symptoms of TSS are nonspecific and often begin with influenza-like symptoms of mild fever and malaise. However, TSS often suddenly advances with symptoms of high fever, nausea, vomiting, diarrhea, skin rash, and a low blood pressure. If it progresses, confusion, headaches, seizures, and skin loss from the palms of the hands and from the soles of the feet can occur. The blood pressure can become dangerously low so that body organs are not profused with enough blood, and if multiorgan failure develops, the patient often dies. The death rate varies widely, depending on how well the patient can respond to treatment. GAS bacteria and Staphylococcus aureus are the predominant bacteria that cause TSS.
How do health care professionals diagnose group A streptococcal (GAS) infections?
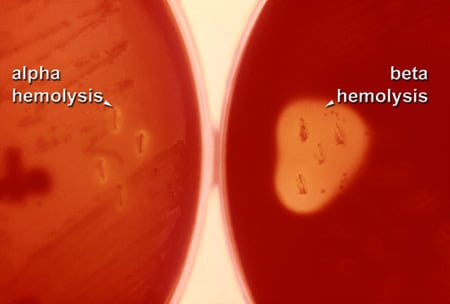
After a history and physical examination, many clinicians presumptively diagnose strep throat from its symptom production and throat appearance (see Fig. 2). However, cultures from the throat or other site of infection form the basis of definitive testing. For example, GAS organisms will grow on sheep blood agar plates that contain two different antibiotics and cause beta hemolysis (complete sheep blood red cell lysis to form a clear area) of the sheep red blood cells (see Fig. 3). In addition, there are rapid tests (RADT or rapid antigen detection test) that take only a few minutes to complete that detect a carbohydrate surface antigen produced by GAS, with specificity of about 95% or better and fairly good sensitivity of about 80%-90%.
Because there are many other groups of Streptococcus spp., positive identification of the infecting bacteria is necessary to separate out other bacteria that may cause some similar symptoms but may require a different workup, different treatment, and produce different complications.
These tests help distinguish GAS from Streptococcus pneumoniae and other organisms.
What is the treatment for invasive group A streptococcal disease?
Antibiotics treat invasive GAS infections as well as noninvasive group A strep infections. Although many antibiotics may be adequate treatment for GAS infections, the best practice methods would be to determine the antibiotic sensitivity of GAS bacteria to be sure the bacteria are susceptible to the antibiotics.
- Milder infections caused by GAS (strep throat, skin infections) are often treated with oral antibiotics (for example, penicillin v [Pen-Vee-K, Veetids], amoxicillin [Amoxil, Dispermox, Trimox], cephalosporins; if allergic to penicillin, erythromycin [E-Mycin, Eryc, Ery-Tab, Pce, Pediazole, Ilosone], azithromycin [Zithromax, Zmax]).
- Some third-generation cephalosporins (for example, ceftriaxone [Rocephin]), given IV or IM, followed by oral antibiotics are useful to treat mild to moderate infections.
- However, invasive group A strep infections require a more aggressive treatment approach. High doses of penicillin, together with clindamycin (Cleocin) by sequential IV administration, are often recommended.
- Some investigators suggest adding immune globulin to the multi-antibiotic treatment.
- In addition to antibiotics, surgical intervention may be necessary to remove dead and dying tissue to limit the spread of invasive GAS organisms. This is almost always done in patients who develop necrotizing fasciitis.
Besides, early diagnosis and treatment of invasive GAS infections yield the best patient outcomes. Many clinicians consult with an infectious disease specialist to help determine the best antibiotic therapy for individual patients. More GAS strains are being reported to have some resistance to one or more antibiotics so the treatment may require alterations in antibiotics. The infectious disease specialist can help choose the most effective antibiotic combinations to treat antibiotic-resistant GAS organisms.
What specialists treat group A streptococcal infections?
The specialists that treat group A streptococcal infections are infectious-disease specialists. However, depending on the severity and the type of infection, other specialists may be involved. For example, if hospitalization is needed, a critical care specialist may join the team; if the person is pregnant, an OB/GYN specialist and/or a pediatric specialist may be needed. If surgical debridement is needed (necrotizing fasciitis), a surgical specialist would be consulted. Other types of medical specialists that may care for patients with GAS infections include emergency-medicine specialists, dermatologists, internal-medicine specialists, family-medicine specialists, nephrologists, and ear, nose, and throat specialists.
What complications are seen with group A streptococcal infections?
Many of the complications of GAS infections are considered to be diseases themselves. For example, scarlet fever, rheumatic fever, necrotizing fasciitis, toxic shock syndrome, and many others can complicate or be triggered by GAS infection. Other post-streptococcal complications can include the necessity to remove tonsils, renal damage, abscess formation, seizures, and other organ damage; some researchers suggest that severe GAS infections in children may lead to permanent or long-lasting brain changes. Although GAS infections in pregnant females during pregnancy and delivery are infrequent, they require immediate treatment to avoid post-streptococcal complications such as endometritis, sepsis, necrotizing fasciitis, or toxic shock syndrome.
Is it possible to prevent group A streptococcal infections?
Many GAS infections can be prevented by reducing the spread of organisms from one person to another. Washing hands frequently is one of the major ways to reduce bacterial transmission. Also, not sharing the same food and drink containers with others may be effective. For those people with a GAS infection, covering the mouth and nose when sneezing or coughing can reduce the chance of transmitting the bacteria to others. Washing material that comes in contact with GAS-infected people is also another way to reduce exposure to GAS organisms.
Early treatment of deep infections (for example, excision, drainage, and antibiotic treatment of rectal abscesses) helps prevent invasive GAS disease. Besides, appropriate and timely removal of tampons and surgical packing may reduce the incidence of toxic shock syndrome.
Currently, there is no vaccine commercially available for GAS, but researchers are working on developing vaccines. At least four different major approaches are being researched. There has been some success with a related experimental vaccine against GAS bacterial antigens coupled to cholera toxin subunits. However, the GAS vaccine, by Vaxent, a vaccine company, prepared by recombinant technology, maybe going into human clinical trials. The new experimental vaccines may become available in the future to prevent GAS infections.
What is the prognosis for group A streptococcal infections?
The prognosis for mild GAS infections is usually good to excellent. The prognosis for patients with chronic diseases, such as diabetes or cancer, or for those who are immunosuppressed, is more guarded, but often is still good with early treatment. However, the prognosis for patients developing necrotizing fasciitis or toxic shock syndrome ranges from good with early effective treatment to poor when the diseases are diagnosed and treated late in the disease process.
Where can people find more information about group A streptococcal infections?
The following sites can provide additional information about GAS infections:
"Strep Throat," MedicineNet.com
"Rapid Strep Test," MedicineNet.com
