Chronic Rhinitis and Post-Nasal Drip
Chronic rhinitis and post-nasal drip definition and facts
- Rhinitis is inflammation of the nose.
- Symptoms of rhinitis include runny nose (rhinorrhea), nasal itching, nasal congestion, and sneezing.
- Rhinitis is categorized into allergic rhinitis (hay fever), non-allergic rhinitis, and mixed rhinitis (a combination of allergic and non-allergic).
- One of the most common characteristics of chronic rhinitis is post-nasal drip, which is mucus accumulation in the back of the nose and throat that drips downward from the back of the nose. Post-nasal drip can cause sore throat, cough, or throat clearing.
- Treatment for rhinitis includes avoiding allergens, medications (both over-the-counter and prescription), and irrigating the nasal passages. Surgery is a last resort to correct any structural issues in the sinuses that may be causing the symptoms.
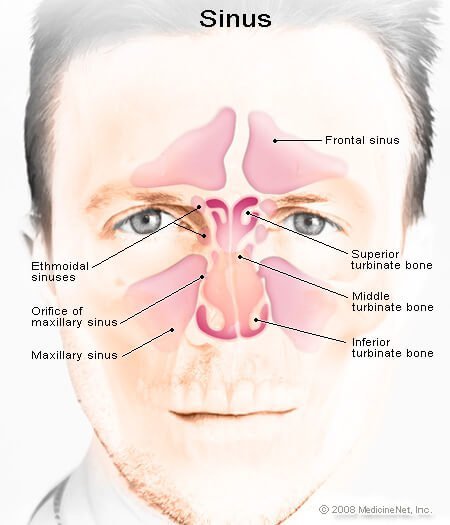
Where are the sinuses, and what do they look like?

The sinuses are air-filled bones in a dense portion of the skull bone, and they decrease the weight of the skull. Four right-left pairs form the sinuses.
What are rhinitis and post-nasal drip? What are the symptoms and signs?
Rhinitis is inflammation of the inner lining of the nose and it has many different causes. Rhinitis is a very common condition. Symptoms include:
- Runny nose (rhinorrhea)
- Nasal itching
- Nasal congestion
- Sneezing
A significant association exists between rhinitis (allergic), asthma, and chronic sinusitis (inflammation of the sinuses for more than 12 weeks) in some individuals. Some evidence suggests that up to 3 of every 5 patients have multiple conditions.
Post-nasal drip is mucus accumulation in the back of the nose and throat leading to, or giving the sensation of, mucus dripping downward from the back of the nose. One of the most common characteristics of chronic rhinitis is post-nasal drip. Post-nasal drip may lead to chronic sore throat, chronic cough, or throat clearing. Post-nasal drip can be caused by excessive or thick mucus secretions or impairment in the normal clearance of mucus from the nose and throat.
What causes rhinitis?
Rhinitis has many possible causes. Rhinitis can be either acute or chronic, and is categorized into three areas: allergic rhinitis, non-allergic rhinitis, and mixed rhinitis (a combination of allergic and non-allergic).
Allergic rhinitis is the most common cause of rhinitis. It is caused by environmental allergies and is characterized by an itchy or runny nose, sneezing, and nasal congestion. Other allergic symptoms include:
- Itchy ears and throat
- Red or watery eyes
- Cough
- Fatigue/loss of concentration/lack of energy from loss of sleep
- Headaches or facial tenderness (not typical)
People with allergic rhinitis also have a higher incidence of asthma and eczema, which are also mainly allergic in origin.
Seasonal allergic rhinitis (hay fever) is usually caused by pollen in the air, and sensitive patients have symptoms during peak times during the year.
Perennial allergic rhinitis, a type of chronic rhinitis is a year-round problem, and is often caused by indoor allergens (particles that cause allergies), such as dust and animal dander in addition to pollens that may exist at the time. Symptoms tend to occur regardless of the time of the year.
Is rhinitis always related to allergies?
No, rhinitis may have many causes other than allergies.
Non-allergic rhinitis occurs in those individuals in whom an allergic or other cause of rhinitis cannot be identified, and the rhinitis occurs for weeks to months at a time for at least a year. These conditions may not have the other allergic manifestations, such as itchy and runny eyes, and are more persistent and less seasonal.
Forms of non-allergic rhinitis include:
- Idiopathic rhinitis often does not have a specific cause identified, but commonly includes upper respiratory infections.
- Vasomotor rhinitis is thought to occur because of abnormal regulation of nasal blood flow and may be induced by temperature fluctuations in the environment, such as cold or dry air, or irritants such as:
- Air pollution
- Smog
- Tobacco smoke
- Car exhaust
- Strong odors such as detergents or fragrances
- Weather conditions (such as the arrival of a weather front)
- Gustatory rhinitis may present predominantly as runny nose (rhinorrhea) related to consumption of hot or spicy food.
- Rhinitis of pregnancy or, generally speaking, hormonal alterations as seen with pregnancy, menopause, and some thyroid changes have been linked to rhinitis.
- Atrophic rhinitis following extensive sinus surgery or from a rare nasal bacterial infection.
- Non-allergic rhinitis with nasal eosinophilia syndrome (NARES) is characterized by a clear nasal discharge. The nasal discharge is found to have eosinophils (allergic cell type), although the patient may not have any other evidence of allergy by skin testing or history or symptoms.
Occupational rhinitis may arise from exposure to irritants at a person's workplace with improvement of symptoms after the person leaves the workplace.
Other causes of rhinitis may be related to:
- Certain medications (oral contraceptives, some blood pressure medications, some anxiety medications, some erectile dysfunction medications, and some anti-inflammatory medications)
- Some nasal structural abnormalities (deviated septum, perforated septum, tumors, nasal polyps, or foreign bodies)

Infections, mostly viral, are a common cause of rhinitis. Viral rhinitis is usually not chronic and may resolve by itself.
Sometimes rhinitis may be related to other generalized medical conditions such as:
- Acid reflux disease (GERD)
- Granulomatosis with polyangiitis
- Sarcoidosis
- Cystic fibrosis
- Other less common conditions
What conditions cause an abnormal production of nasal secretions?
The following conditions are often associated with increased nasal drainage (runny nose). It is common to have more than one factor involved in a particular individual.
- Viruses
- Allergies
- Cold temperatures
- Certain foods or spices
- Pregnancy or hormonal changes
- Drug side-effects (particularly certain high blood pressure medications)
- Structural problems (deviated septum, large turbinates)
- Vasomotor rhinitis (an abnormal regulatory problem with the nose)
Decreasing the fluid content of the mucus usually thickens the secretions leading to the impression of increased mucus. The following may cause thickened secretions:
- Low humidity
- Sinus or nasal infections
- Foreign bodies (especially if the drainage is from one side)
- Environmental irritants (tobacco smoke, smog)
- Structural problems (deviated septum, enlarged turbinates, enlarged adenoids)
- Advanced age -- mucus membrane lining the nose can shrink with age leading to a reduced volume of secretions that are thicker
- Hormonal problems
- Drug side effects (antihistamines)
What conditions cause an impaired clearance of nasal secretions?
The primary reason for impaired clearance of nasal secretions within the nasal cavities is from smoking. Smoking impairs the movement of the cilia (microscopic hairs) and their ability to push the secretions out of the nasal cavity to be swallowed. Other conditions that can impact clearance of secretions in the nose include allergies and some genetic disorders.
Swallowing problems can make it difficult to clear normal secretions from the back of the throat. This may result in the accumulation of material in the throat, which can spill into the voice box, causing hoarseness, throat clearing, or cough. The following factors can contribute to swallowing problems:
- Advancing age: This will lead to decreased strength and coordination in swallowing.
- Stress: Stress leads to muscle spasm or "lump in throat." A nervous habit of frequent throat clearing also will make the condition worse.
- Narrowing of the throat due to tumors or other conditions: This will impair the passage of food.
- Gastroesophageal reflux disease (GERD)
- Nerve or muscle disorders: (stroke, and muscle diseases, etc.)
Which specialties of doctors treat chronic rhinitis and post-nasal drip?
- A primary care provider (PCP) such as a family practitioner, an internist, or a child's pediatrician may diagnose chronic rhinitis and post-nasal drip. If chronic rhinitis and post-nasal drip are due to allergies you may see an allergist/immunologist.
- If chronic rhinitis and post-nasal drip are due to asthma, you may see a pulmonologist, a specialist in conditions affecting the lungs.
- If the conditions are severe or recurrent, you may be referred to an otolaryngologist, also called an ear-nose-throat (ENT) specialist, for further treatment.
- If you get chronic rhinitis and post-nasal drip during pregnancy, you may be referred to your obstetrician/gynecologist (OB/GYN).
- If acid reflux disease (GERD) is the cause of your chronic rhinitis and post-nasal drip, you may see a gastroenterologist, a specialist in conditions of the digestive tract.
How can chronic rhinitis and post-nasal drip be treated?
The treatment generally is directed toward the underlying cause.
Identifying and avoiding allergens
An allergy is an exaggerated "normal body" inflammatory response to an outside substance. These substances that cause allergies are called allergens, and typically include:
The best treatment is avoidance of these allergens, but in many cases this may be very difficult if not impossible. Some helpful suggestions include:
- Use a pollen mask when mowing the grass or cleaning the house.
- Install an air purifier or at least change the air filters monthly in heating and air conditioning systems.
- Use cotton or synthetic materials such as Dacron in pillows and bedding.
- Enclose mattress in plastic.
- Select dust-mite proof pillow covers.
- Consider using a humidifier.
- Keep windows closed during high pollen times.
- Eliminate house plants.
- Bathe pets frequently or do not adopt or purchase dander-producing pets.
Avoidance of nasal irritants: Nasal irritants usually do not lead to the typical immune response seen with classical allergies, but nevertheless they can mimic or make allergies worse, as in vasomotor rhinitis. Examples of these irritants include cigarette smoke, perfume, aerosol sprays, smoke, smog, and car exhaust.
A health care professional may identify possible allergens by taking a very careful history. Details of the patient's possible exposure to allergens or irritants at home or the workplace may give clues. An allergy specialist (allergy and immunologist) can perform skin tests to try to identify common environmental allergies.
What medications can be used to treat rhinitis and post-nasal drip?
In addition to measures noted above, medications may also be used for the treatment and relief of rhinitis and post-nasal drip.
For allergic rhinitis and post-nasal drip, many medications are used. It also is essential to attempt to avoid the offending allergic particles.
Steroid nasal sprays
Intra-nasal glucocorticoids (steroid sprays applied directly into the nose) are often recommended as the first line of treatment. Steroids are potent anti-inflammatory and anti-allergic agents and may relieve most of the associated symptoms of runny and itchy nose, nasal congestion, sneezing, and post-nasal drip.
Their use must be monitored and tapered by the prescribing physician, as long-term use may have significant side effects. Examples of the nasal steroids include:
- beclomethasone (Beconase, Beconase AQ, Vancenase, Vancenase AQ)
- flunisolide (Nasarel, Nasalide)
- budesonide (Rhinocort)
- fluticasone propionate (Flonase)
- mometasone furoate (Nasonex)
- fluticasone furoate (Veramyst)
- triamcinolone (Nasacort)
- ciclesonide (Omnaris, Zetonna)
- acetonide (Tri-Nasal)
These are generally used once or twice daily. Tilt the head forward during administration to avoid spraying the back of the throat instead of the nose.
Oral steroids
These drugs -- for example, prednisone, methylprednisolone (Medrol), and hydrocortisone (Hydrocortone, Cortef) -- are highly effective in allergic patients. They are best used for short-term management of allergic problems, and a health care professional must always monitor their use, as there are potential serious side effects when using these medications for extended periods. These are reserved only for very severe cases that do not respond to the usual treatment with nasal steroids and antihistamines.
Antihistamines
Allergy medications such as antihistamines are also frequently used to treat allergic rhinitis and post-nasal drip. These are generally used as the second line of treatment after the nasal steroids or in combination with them. Histamines are naturally occurring chemicals released in response to an exposure to an allergen, which are responsible for the congestion, sneezing, and runny nose typical of an allergic reaction. Antihistamines are drugs that block the histamine reaction. These medications work best when given prior to exposure.
Antihistamines can be divided into two groups:
- Sedating, or first generation, for example, diphenhydramine (Benadryl), chlorpheniramine (Chlor-Trimeton), clemastine (Tavist). Sedating antihistamines should be avoided in those patients who need to drive or use dangerous equipment.
- Non-sedating or second generation, for example, loratadine (Claritin), cetirizine (Zyrtec),fexofenadine (Allegra). Non-sedating antihistamines can have serious drug interactions. Most of these are found over the counter.
There is a nasal antihistamine preparation that has been shown to be very effective in treating allergic rhinitis, called azelastine nasal (Astelin).
Decongestant sprays
Examples of decongestant sprays include:
- oxymetazoline (Afrin, Dristan)
- phenylephrine (Neo-Synephrine)
Decongestant sprays quickly reduce swelling of nasal tissues by shrinking the blood vessels. They improve breathing and drainage over the short-term, and their use should be limited to 3 to 5 days because of the potential for rebound addiction. If they are used for more than a few days, they can become highly addictive (rhinitis medicamentosa). Long-term use can lead to serious damage.
Oral decongestants
Oral decongestants temporarily reduce swelling of sinus and nasal tissues leading to an improvement of breathing and a decrease in obstruction. They may also stimulate the heart and raise the blood pressure and should be avoided by patients who have high blood pressure, heart irregularities, glaucoma, thyroid problems, or difficulty in urination. The most common decongestant is pseudoephedrine (Sudafed).
Cromolyn sodium (Nasalcrom)
Cromolyn sodium (Nasalcrom) is a spray that helps to stabilize allergy cells (mast cells) by preventing release of allergy mediators, like histamine. They are most effective if used before the start of allergy season or prior to exposure to a known allergen.
Montelukast (Singulair)
Montelukast (Singulair) is an agent that acts similarly to antihistamine, although it is involved in another pathway in allergic response. Research shows it to be less beneficial than the steroid nasal sprays, but equally as effective as some of the antihistamines. It may be useful in patients who do not wish to use nasal sprays or those who have co-existing asthma.
Ipratropium (Atrovent nasal)
Ipratropium (Atrovent nasal) is used as a nasal spray and helps to control nasal drainage mediated by neural pathways. It will not treat an allergy, but it does decrease nasal drainage.
Mucus thinning agents
Mucus thinning agents are utilized to make secretions thinner and less sticky. They help to prevent pooling of secretions in the back of the nose and throat where they often cause choking. The thinner secretions pass more easily. Guaifenesin (Humibid, Fenesin, Organidin) is a commonly used formulation. If a rash develops or there is swelling of the salivary glands, this medication should be discontinued. Inadequate fluid intake will also thicken secretions. Drinking more water, eliminating caffeine from the diet, and avoiding diuretics can help.
Immunotherapy
Immunotherapy treatment has a goal of reducing a person's response to an allergen. After identification of an allergen, small amounts are given back to the sensitive patient. Over time, the patient will develop blocking antibodies to the allergen and will become less sensitive and less reactive to the substance causing allergic symptoms. The allergens are given in the form of allergy shots or by delivery of the allergen under the tongue (sublingual therapy). Sublingual therapy has been more common in Europe. In either method, the goal is to interfere with the allergic response to specific allergens to which the patient is sensitive.
Combinations
These drugs are made up of one or more anti-allergy medications. They are usually a combination of an antihistamine and a decongestant. Other common combinations include mucus thinning agents, anti-cough agents, aspirin, ibuprofen (Advil), or acetaminophen (Tylenol). They help to simplify dosing and often will work either together for even more benefit or have counteracting side effects that eliminate or reduce total side effects.
There are some combination nasal preparations available as well to target the tissue of the nose. The combination of azelastine and fluticasone (Dymista) combines a nasal antihistamine and steroid to help provide relief of seasonal allergic rhinitis symptoms.
What can be used to treat non-allergic rhinitis?
Treatment of non-allergic rhinitis is similar to the treatment of allergic rhinitis.
Steroid nasal sprays and nasal antihistamines, for example, azelastine (Astelin) as described in more detail in the previous section, are the mainstay of therapy for non-allergic rhinitis. Combination therapy using steroid nasal spray and nasal antihistamine has been shown to be more beneficial.
The other therapies, such as ipratropium (Atrovent) and decongestants, also may be used in patients who continue to have symptoms despite proper therapy with nasal steroids and nasal antihistamines.
Does salt water or nasal irrigation have any role in the treatment of rhinitis and post-nasal drip?
Irrigating the nose with salt water is a home remedy that is very useful therapy for non-allergic rhinitis, and especially beneficial for treatment and relief of post-nasal drip.
Nasal irrigation utilizing a buffered isotonic saline solution (salt water) helps to reduce swollen and congested nasal and sinus tissues. In addition, it washes out thickened nasal secretions, irritants (smog, pollens, etc.), bacteria, and crusts from the nose and sinuses. Non-prescription nasal sprays (Ocean spray, Ayr, Nasal) can be used frequently and are very convenient to use.
- Nasal irrigation can be done several times per day.
- Nasal irrigation is frequently performed with a syringe, a Waterpik device (the attachment is purchased separately), or a Neti pot.
- The irrigating solution can be made by adding two to three heaping teaspoons of non-iodized (does not sting) salt to one pint of room-temperature distilled water. It is best to use Morton Coarse Kosher Salt or Springfield plain salt because table salt may have unwanted additives. To this solution, add one teaspoon of baking soda.
- Store at room temperature, and always mix the solution before each use.
- If the solution stings, use less salt.
- In the beginning, or for children, it is best to start with a weaker salt mixture. It is not unusual to initially have a mild burning sensation the first few times you irrigate.
- While irrigating the nose, it is best to stand over the sink and irrigate each side of your nose separately. Aim the stream toward the back of your head, not at the top of your head.
- For young children, the salt water can be put into a small spray container, which can be squirted many times into each side of the nose.
What are other options for the treatment of rhinitis and post-nasal drip?
Treatment can also be directed toward specific causes of rhinitis and post-nasal drip as outlined below.
Treatment of infection
The most common nasal infection is a viral infection known as "the common cold." The virus causes swelling of the nasal membranes and production of thick clear mucus. Symptoms usually last several days. If "a cold" goes on for many days and is associated with yellow or green drainage, a secondary bacterial infection is suspected. Very few patients with a common cold from a virus will go on to have acute bacterial rhinosinusitis from sinus blockage and impaired sinus function. Sinus blockage can lead to acute sinusitis (less than 4 weeks in duration) or chronic sinusitis (lasting 12 weeks with continuous symptoms), which can be characterized by nasal congestion, thick mucus, and facial or dental pain. From 4 to 12 weeks, the symptoms are classified as subacute sinusitis or recurrent acute sinusitis.
Symptomatic treatment often involves pain relief, decongestants, mucous thinning medications, saline rinses, and antihistamine therapy.
Reflux Medications
For rhinitis that is a result of acid reflux disease, antacids (Maalox, Mylanta) can help to neutralize acid contents, whereas other medications such as cimetidine (Tagamet), famotidine (Pepcid), omeprazole (Prilosec), esomeprazole (Nexium) can decrease stomach acid production. Non-pharmacological treatments include avoiding late evening meals and snacks and eliminating alcohol and caffeine. Elevating the head of the bed may help decrease reflux during sleep.
Surgery
Structural problems with the nose and sinuses may ultimately require surgical correction to cure them. This should be done only after more conservative measures have been tried and failed. Septal deviation, septal spurs, septal perforation, enlargement of the turbinates, and nasal/sinus polyps can lead to pooling of or overproduction of secretions, blockage of the normal pathways leading to chronic sinusitis, and chronic irritation. An ear-nose-throat doctor (otolaryngologist) performs the surgery. Surgery can also enhance the delivery of nasal medications and rinses into the nasal cavities.
