Ulcerative gingivitis
Understanding Ulcerative Gingivitis (ANUG/NUG)
Ulcerative gingivitis, commonly known as Acute Necrotizing Ulcerative Gingivitis (ANUG) or simply Necrotizing Ulcerative Gingivitis (NUG), is a distinct and painful infectious disease of the gums (gingiva). It is characterized by acute inflammation accompanied by necrosis (tissue death) and ulceration of the gingival tissues, particularly the interdental papillae (the gum tissue between teeth).
Pathogenesis and Etiology
The underlying pathogenesis of ulcerative gingivitis involves a complex interplay of factors, with a predominant role of tissue alteration processes (necrosis) driven by a specific bacterial infection in a susceptible host. The key etiological factors include:
- Bacterial Infection: The primary causative agents are believed to be an overgrowth of a specific complex of anaerobic bacteria, notably fusiform bacteria (e.g., *Fusobacterium nucleatum*) and spirochetes (e.g., *Treponema vincentii*, *Prevotella intermedia*). This is often referred to as a fusospirochetal infection. These microorganisms are often part of the normal oral microflora but can become pathogenic under certain conditions.
- Impaired Host Resistance: A crucial factor is a decrease in the resistance of the gingival mucosa and the host's overall immune response. Predisposing factors that lower host resistance include:
- Stress: Psychological or physiological stress.
- Poor Oral Hygiene: Accumulation of plaque and calculus creates an environment conducive to bacterial overgrowth.
- Smoking: A significant risk factor.
- Malnutrition: Particularly deficiencies in vitamins C and B complex.
- Systemic Diseases: Conditions that compromise the immune system, such as HIV/AIDS, leukemia, or immunosuppressive therapy.
- Pre-existing Gingivitis: Chronic gingival inflammation can predispose to ANUG.
- Lack of Sleep and Fatigue.
In the clinical setting of dental practice, ulcerative gingivitis typically presents in its acute form (ANUG). While chronic forms or progression to more severe necrotizing periodontal diseases (NUP) can occur, the initial presentation is usually acute and intensely symptomatic.
Symptoms and Diagnosis of Ulcerative Gingivitis
Clinical Presentation
The clinical picture of ulcerative gingivitis (ANUG) is quite typical and is characterized by an acute and painful onset. Patients commonly complain of:
- Intense Gingival Pain: Often spontaneous and severe, making eating and oral hygiene difficult.
- Gingival Bleeding: Gums bleed easily, even with slight provocation or spontaneously.
- Putrid Breath (Fetid Halitosis): A characteristic foul odor due to tissue necrosis and bacterial activity.
- Metallic Taste: Some patients report an unpleasant metallic taste.
- Increased Salivation.
Systemic manifestations are also common in patients with ulcerative gingivitis:
- Malaise and Weakness: A general feeling of being unwell.
- Fever: Body temperature may rise, sometimes significantly.
- Headache.
- Decreased Performance/Lethargy.
- Loss of Appetite.
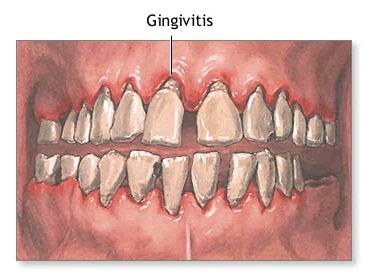
Upon examination of the oral cavity, the following findings are characteristic of ANUG:
- Necrotic Ulcerations: The gingival margin, especially the interdental papillae, is covered with a grayish, easily removable pseudomembrane or slough (fetid plaque). Removal of this plaque exposes a raw, bleeding, and sharply painful ulcerated surface.
- "Punched-Out" Papillae: The tips of the interdental papillae appear cratered or "punched out" due to necrosis, and the normal contours of the gingival margin are broken or blunted.
- Erythema and Edema: The surrounding gingiva is often intensely red and swollen.
- Poor Oral Hygiene: Patients typically have abundant non-mineralized dental deposits (plaque) and often "tartar" (calculus).
- Regional Lymphadenopathy: The submandibular and sometimes posterior auricular (behind the ear) lymph nodes may be enlarged and painful on palpation.
Diagnostic Evaluation
During the acute period of ulcerative gingivitis, the diagnostic process involves:
- Patient Interrogation (History): Detailed medical and dental history, including onset and nature of symptoms, predisposing factors (stress, smoking, recent illness, poor oral hygiene).
- Clinical Examination: Thorough intraoral examination to assess the characteristic gingival lesions, extent of necrosis, presence of plaque/calculus, and halitosis.
- Palpation of Regional Lymph Nodes.
- Measurement of Body Temperature.
- Laboratory Tests (if systemic involvement is significant):
- Complete Blood Count (CBC): May reveal leukocytosis (increased white blood cell count) and an increase in the erythrocyte sedimentation rate (ESR), indicating systemic inflammation.
- Urinalysis: Protein may occasionally be found in the urine of patients with severe systemic effects of ulcerative gingivitis.
- Microbiological Smears (less common for routine diagnosis): While characteristic fusospirochetal bacteria are involved, diagnosis is usually clinical. Smears are not typically needed unless the presentation is atypical or unresponsive to initial treatment.
After the acute inflammatory phenomena of ulcerative gingivitis have subsided, it is advisable to conduct an in-depth examination of the patient. This aims to identify and address any underlying reasons for the decrease in the body's resistance and the development of the disease (e.g., nutritional deficiencies, systemic conditions, chronic stress, ongoing poor oral hygiene) to prevent recurrence.
Treatment of Ulcerative Gingivitis
The treatment of ulcerative gingivitis (ANUG) should be initiated promptly and actively, ideally at the patient's first visit to the dentist or periodontist. With correct and timely management, patients often experience significant improvement within 12-24 hours.
The treatment goals are to alleviate pain, control the acute infection, remove necrotic tissue and local irritants, and address underlying predisposing factors to prevent recurrence.
Initial (Acute Phase) Management - Typically by a Dental Professional
- Anesthesia: Local anesthesia is performed on the gum areas affected by ulcerative gingivitis to allow for comfortable debridement. Topical anesthetics applied via applications or gentle oral baths with 0.5-2% solutions of novocaine (procaine), lidocaine, or another suitable local anesthetic are often used initially.
- Debridement of Necrotic Tissue: Gentle but thorough removal of the necrotic gingival tissue (pseudomembrane and slough) is essential. This can be done with cotton pellets soaked in hydrogen peroxide, curettes, or ultrasonic scalers. Application of proteolytic enzymes (e.g., chymopsin, chymotrypsin - historical mention) to the gums was thought to aid in dissolving necrotic tissue, but mechanical debridement is primary. The aim should be to remove all visible necrotic plaque from the gums during the first visit.
- Removal of Local Irritants: Gross dental deposits (plaque and calculus, "tartar") are carefully removed. Any sharp edges of teeth or restorations that may be injuring the mucous membrane are smoothed off.
- Antimicrobial Irrigation/Application: After cleansing the gums of necrotic masses, topical antimicrobial agents are applied. This can include:
- Irrigation or gentle rinsing with 0.12% chlorhexidine gluconate solution (modern standard) or historically 1% hydrogen peroxide solution.
- Application of metronidazole suspension or gel directly to the affected areas.
- Sanguinarine-containing products (herbal antiseptic, less common now).
Home Care and Systemic Medications (Prescribed by Dentist/Physician)
Therapeutic measures for patients with ulcerative gingivitis to follow at home typically include:
- Systemic Antibiotics: Metronidazole (e.g., 250-500 mg 2-3 times a day) is often the antibiotic of choice due to its effectiveness against anaerobic bacteria. Penicillin or amoxicillin may also be used.
- Analgesics/Anti-inflammatories: Acetylsalicylic acid (aspirin - use with caution in certain populations) (e.g., 0.5 g up to 3 times a day) or other NSAIDs like ibuprofen for pain and inflammation.
- Antihistamines (if significant swelling or allergic component suspected): Diphenhydramine (e.g., 0.05 g each morning and evening) was historically used, though less common now for this specific indication unless allergy is a factor.
- Antiseptic Mouth Rinses: Frequent gentle rinsing with antiseptic solutions such as 0.12% chlorhexidine gluconate, dilute hydrogen peroxide (e.g., 1.5%), or historically, furacilin. Warm saline rinses are also beneficial.
- Herbal Decoctions: Rinsing with decoctions of herbs like chamomile, sage, or calendula for their mild anti-inflammatory and soothing properties.
- Supportive Measures:
- Plentiful fluid intake.
- A soft, nutritious, non-irritating diet (avoiding spicy, acidic, or hard foods).
- Avoidance of smoking and alcohol.
- Stress reduction.
Subsequent (Healing Phase) Management - By Dental Professional
From the second visit onwards, as the patient's general condition and local oral status improve, treatment focuses on promoting healing and tissue regeneration:
- Continued gentle debridement if needed.
- Applications of agents that promote epithelization of ulcerated surfaces. Examples include:
- Sea buckthorn oil or rosehip oil.
- Carotolin (a carotenoid-rich preparation).
- Solcoseryl (a deproteinized calf blood extract - use varies by region).
- Oil solutions of vitamins A and E.
- Actovegin (another deproteinized hemodialysate - use varies).
Comprehensive Oral Rehabilitation
After the acute inflammation of ulcerative gingivitis is relieved, thorough debridement of the oral cavity is performed. This includes:
- Complete scaling and root planing to remove all remaining plaque and calculus.
- Correction of any plaque-retentive factors (e.g., overhanging restorations, poorly fitting prostheses).
- Comprehensive oral hygiene instruction and reinforcement.
- Addressing any underlying predisposing factors (e.g., nutritional counseling, stress management referral, smoking cessation).
- Gingival contouring (gingivoplasty) may be necessary in some cases after healing if "punched-out" craters persist, to restore normal gingival architecture and prevent plaque accumulation.
Long-term follow-up is important to monitor gingival health and prevent recurrence.
Differential Diagnosis of Acute Gingival Lesions
Ulcerative gingivitis must be differentiated from other conditions that can cause acute gingival inflammation, ulceration, or pain:
| Condition | Key Differentiating Features |
|---|---|
| Acute Necrotizing Ulcerative Gingivitis (ANUG/NUG) | Sudden onset, severe pain, interdental papillary necrosis ("punched-out"), pseudomembrane formation, fetid odor, gingival bleeding, often systemic symptoms (fever, malaise). Associated with stress, smoking, poor hygiene, specific bacteria. |
| Herpetic Gingivostomatitis (Primary Herpes Simplex) | Often in children; multiple painful vesicles that rupture to form shallow, round ulcers on gingiva, lips, tongue, buccal mucosa. Diffuse gingival erythema and edema. Fever, malaise, lymphadenopathy common. Viral etiology. |
| Aphthous Ulcers (Canker Sores) | Discrete, recurrent, painful, round/oval ulcers with erythematous halo and yellowish-gray base. Typically on non-keratinized mucosa (buccal, labial, tongue, floor of mouth), less commonly solely on attached gingiva. No generalized gingival necrosis. |
| Erythema Multiforme | Acute mucocutaneous condition; can involve oral mucosa with painful erosions/ulcers, often hemorrhagic crusting of lips. Target lesions on skin may be present. Triggered by infections or drugs. |
| Pemphigus Vulgaris / Mucous Membrane Pemphigoid | Autoimmune blistering diseases. Oral lesions often present as desquamative gingivitis, erosions, or intact bullae that rupture. Nikolsky's sign may be positive. Biopsy and immunofluorescence needed. |
| Agranulocytosis / Leukemia | Can present with severe oral ulcerations, necrosis, and gingival bleeding due to immunosuppression and neutropenia. Systemic signs of illness, abnormal blood counts. (May involve severe forms of gingivitis or periodontitis). |
| Desquamative Gingivitis (Symptom complex) | Intensely red, peeling, friable gingiva. Can be a manifestation of lichen planus, pemphigoid, pemphigus, or other conditions. Less often presents with acute punched-out ulcers like ANUG. (This is a descriptive term, not a single disease, but relates to gingival inflammation which is covered under Periodontal disease). |
Complications and Predisposing Factors
If ANUG is not treated promptly or if host resistance is severely compromised, the infection can progress to more severe forms of necrotizing periodontal disease:
- Necrotizing Ulcerative Periodontitis (NUP): Involves destruction of the periodontal ligament and alveolar bone, leading to tooth mobility and loss.
- Necrotizing Stomatitis: Spread of necrosis to involve broader areas of oral mucosa beyond the gingiva.
- Noma (Cancrum Oris): A rare, devastating gangrenous infection that can spread rapidly to destroy facial tissues, primarily seen in severely malnourished children in impoverished regions.
Recurrence of ANUG is possible if underlying predisposing factors (poor oral hygiene, smoking, stress, systemic conditions) are not adequately addressed.
Prevention and When to Seek Dental Care
Prevention of ulcerative gingivitis centers on:
- Maintaining Good Oral Hygiene: Regular and effective brushing, flossing, and interdental cleaning to control plaque.
- Regular Dental Check-ups and Cleanings: Professional removal of calculus and plaque.
- Healthy Lifestyle: Balanced nutrition, adequate sleep, stress management.
- Smoking Cessation.
- Management of Systemic Conditions: Proper medical care for any underlying diseases that compromise immunity.
It is important to seek **prompt dental care** if you experience symptoms of ulcerative gingivitis, such as:
- Sudden onset of severe gum pain.
- Bleeding gums, especially with a foul odor.
- Grayish film on the gums or ulcerations between teeth.
- Fever or general malaise accompanying these oral symptoms.
Early diagnosis and treatment by a dentist or periodontist are crucial to alleviate pain, control the infection, prevent tissue destruction, and avoid recurrence.
References
- Rowland RW. Necrotizing ulcerative gingivitis. Ann Periodontol. 1999 Dec;4(1):65-73; discussion 78.
- Loesche WJ, Syed SA, Laughon BE, Stoll J. The bacteriology of acute necrotizing ulcerative gingivitis. J Periodontol. 1982 Apr;53(4):223-30.
- Novak MJ. Necrotizing ulcerative periodontitis. Ann Periodontol. 1999 Dec;4(1):74-8; discussion 78.
- Johnson BD, Engel D. Acute necrotizing ulcerative gingivitis. A review of diagnosis, etiology and treatment. J Periodontol. 1986 Mar;57(3):141-50.
- Herrera D, Roldán S, Sanz M. The Porphyromonas gingivalis-Prevotella intermedia-Treponema denticola-Fusobacterium nucleatum complex in patients with adult periodontitis. J Clin Periodontol. 2000 Mar;27(3):213-8. (Context for implicated bacteria)
- American Academy of Periodontology. Glossary of Periodontal Terms. 4th ed. Chicago: American Academy of Periodontology; 2001.
- Newman MG, Takei HH, Klokkevold PR, Carranza FA. Carranza's Clinical Periodontology. 13th ed. Elsevier; 2019. (Standard textbook reference)
See also
- Dental anatomy
- Dental caries
- Periodontal disease:
- Chronic catarrhal gingivitis
- Chronic generalized periodontitis of moderate severity
- Chronic hypertrophic gingivitis
- Chronic mild generalized periodontitis
- Idiopathic periodontal disease, periodontomas
- Periodontitis
- Periodontitis in remission
- Periodontosis
- Severe chronic generalized periodontitis
- Ulcerative gingivitis