Endoscopic Treatment of Ulnar Nerve Compression in the Ulnar Canal (Guyon's Canal Syndrome)
Endoscopic treatment of ulnar nerve compression in the ulnar canal (Guyon's canal syndrome)
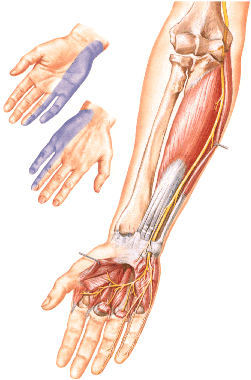
Syndrome of compression of the ulnar nerve in the ulnar canal (Guyon's canal syndrome), along with cubital canal syndrome, is one of the most common syndromes of peripheral nerve compression. Narrowing of the nerve in the ulnar groove occurs for a variety of reasons. Such causes, which cannot be eliminated by external neurolysis in the soft tissue area, require additional ventral nerve displacement.
This is done, for example, in the case of a detected tendency for the nerve to luke out of the groove or in case of bone anatomical changes. In both cases, first, open neurolysis is followed by ventral displacement. In all cases, endoscopic external neurolysis can be performed through one approach, two centimeters long.
After the application of the hemostatic tourniquet, a skin incision about two centimeters long in projection onto the ulnar nerve can be performed. In this case, the nerve is located and marked with a rubber lead. This is followed by the formation of a subcutaneous pocket through which the retractor moves distally and proximally relative to the incision. After inserting the optics, the surgeon obtains a clear image of the anatomy and can perform neurolysis using endoscopic scissors. Due to the optical magnification effect, accidentally dissected blood vessels are clearly visible and therefore coagulated in a targeted manner. The nerve branches are also clearly represented and therefore cannot be injured.
Intra- and postoperative course in the treated patients developed without complications, and the results show, with insignificant postoperative morbidity, a good involution of the symptoms of complications. Immobilization of the operated limb in a cast can be avoided without any problems. The negative effects associated with scarring have not yet been established.
Minimally invasive treatment of peripheral nerve compression opens up the possibility of achieving a functional advantage through scar reduction compared to the conventional method. The elimination of the need for plaster immobilization of the operated limb, as well as the prevention of scar formation in the load zone of the operated limb, ensure early mobilization and restoration of function. Atraumatic preparation in the direction of the nerve can reduce postoperative morbidity and symptoms of complications. The duration of the operation, meanwhile, is no longer than with the traditional method, and the percentage of complications was less.