Aspiration-ultrasonic intracaneal turbinoplasty for nasal septum deviation complicated by inferior turbinate hypertrophy
- Addressing Chronic Nasal Congestion: The Role of Inferior Turbinate Pathology
- Evolution of Inferior Turbinate Correction Techniques
- Aspiration-Ultrasonic Intracavitary Turbinoplasty: A Novel Approach
- Conclusion: Advancing Functional Nasal Surgery
- Differential Diagnosis of Chronic Nasal Congestion
- When to Consider Turbinoplasty
- References
Addressing Chronic Nasal Congestion: The Role of Inferior Turbinate Pathology and Aspiration-Ultrasonic Intracavitary Turbinoplasty
Chronic nasal congestion is a prevalent complaint that significantly impacts quality of life. A common underlying cause is pathology of the inferior turbinates, often exacerbated by or coexisting with conditions like nasal septum deviation. This article focuses on a specific surgical technique, aspiration-ultrasonic intracavitary turbinoplasty, designed to address inferior turbinate hypertrophy in the context of such combined pathology.
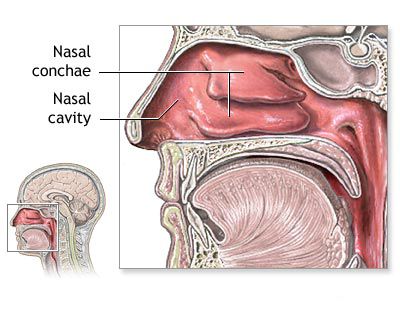
The Importance of Physiological Nasal Breathing
The act of nasal breathing is a complex physiological process, not merely a passive conduit for air. The nature of airflow through the nasal cavity is largely influenced by the structure and function of the inferior turbinates. These structures are responsible for humidifying, warming, and filtering inhaled air, as well as regulating nasal airflow resistance. Physiological nasal breathing is essential for overall respiratory health, proper sleep, and even craniofacial development. Chronic nasal obstruction leading to persistent mouth breathing can have numerous adverse consequences.
Goals of Sparing Surgery for Chronic Nasal Congestion
The primary goal of any surgical intervention for chronic nasal congestion due to turbinate hypertrophy should be to alleviate the patient's complaints (primarily obstruction) while meticulously preserving or restoring normal nasal function. This includes maintaining adequate inspiratory resistance, which is crucial for proper lung mechanics (the "resistor function" of the nose), and ensuring appropriate airflow patterns for optimal air conditioning (the "diffuser function"). Minimally invasive technologies are key to achieving these goals when addressing hypertrophic rhinitis by correcting the inferior turbinates.
Evolution of Inferior Turbinate Correction Techniques
A multitude of surgical techniques have been developed over the years for correcting hypertrophied inferior turbinates causing chronic nasal congestion.
Limitations of Traditional Destructive Methods
Historically, methods such as aggressive conchotomy (partial or total surgical removal of the turbinate), galvanocautery (surface electrocautery), and extensive cryodestruction (freezing) of the inferior turbinates were employed. However, these approaches are now largely considered unacceptable by many specialists due to their destructive nature. Such procedures often result in a significant loss of functional mucous membrane, thereby impairing the essential excretory (mucus production), transport (mucociliary clearance), and absorption functions of the nose. A serious potential long-term consequence of overly aggressive turbinate reduction is the development of atrophic rhinitis or "empty nose syndrome," characterized by chronic dryness, crusting, paradoxical obstruction, and pain.
Modern Sparing (Mucosa-Preserving) Techniques
Therefore, for the correction of hypertrophied inferior turbinates associated with chronic nasal congestion, current best practice emphasizes **sparing, mucosa-preserving methods**. These techniques aim to reduce the bulk of the turbinate, primarily by targeting the submucosal erectile tissue (cavernous plexus) while leaving the overlying respiratory epithelium intact. Common sparing techniques include:
- Submucosal Vasotomy/Excision: Involves creating an incision and then reducing or ablating the submucosal blood vessels and erectile tissue, often from the side of the underlying bone.
- Lateroconchopexy (Turbinate Lateralization): The bony base of the inferior turbinate is fractured and displaced laterally to widen the nasal airway. This is often performed in conjunction with a submucosal reduction technique.
- Submucosal Diathermocoagulation or Radiofrequency Ablation: Uses heat generated by electrical current or radio waves delivered via a probe inserted into the submucosa to shrink the erectile tissue.
- Cavernosotomy: Creating openings into the cavernous tissue to reduce its volume.
- Submucosal Cryodestruction: A more controlled application of cold to the submucosal tissues.
- Powered Instrumentation (Microdebrider or Shaver-Assisted Turbinoplasty): Allows for precise submucosal tissue removal through small incisions.
While these proposed methods of surgical treatment for chronic nasal congestion are generally minimally invasive, some can still have a degree of negative destructive effect on the mucous membrane if not performed meticulously or if too aggressive.
Aspiration-Ultrasonic Intracavitary Turbinoplasty: A Novel Approach
The ongoing development of new, more gentle, and functionally oriented surgical interventions for the treatment of chronic nasal congestion remains a priority. Aspiration-ultrasonic intracavitary turbinoplasty is presented as a technique that aims to reduce the volume of the turbinates without significantly injuring the overlying mucous membrane, thereby preserving its physiological functions.
Rationale and Advantages
This technique utilizes ultrasonic energy for tissue reduction and aspiration to remove debris simultaneously. The goal is to achieve effective turbinate volume reduction while minimizing thermal damage and preserving the mucosal surface, which is critical for normal nasal function. The most indicative measure of success is the dynamic restoration of the respiratory function of the nose after surgery.
Patient Cohort and Anesthesia
A reported series involved 13 patients aged 9 to 15 years who underwent this procedure. The operation is performed under anesthesia (details of the specific anesthetic technique, whether local or general, are noted as "developed by us") using a specialized aspiration-ultrasound device.
Operative Course of Aspiration-Ultrasonic Intracavitary Turbinoplasty
The procedure is described as follows:
- The aspiration-ultrasonic device is used to perform **submucosal intracavitary turbinoplasty** on the inferior (and sometimes middle, if indicated) turbinates. This technique aims to reduce the volume of the turbinates from within, without damaging the surface mucous membrane.
- The objective is to restore the lumen of the common nasal passage to its normal dimensions, thereby eliminating obstacles in the path of airflow and improving nasal aerodynamics.
- If performed in conjunction with septoplasty (for a deviated nasal septum), thin silicone tube inserts (splints) may be placed along the nasal septum to prevent synechiae (adhesions) between the septum and the turbinates.
- Anterior nasal packing with an oil-based ointment is typically applied for one day.
Postoperative Management and Outcomes
According to reported experiences, no significant complications occurred during surgery or in the subsequent treatment period with this technique. Notably, none of the patients in the described series developed synechiae, and nasal breathing was reportedly fully restored. Patients were typically discharged on average 2-3 days after the operation.
Conclusion: Advancing Functional Nasal Surgery
The newly developed technologies of minimally invasive endonasal intracavitary turbinoplasty, particularly when utilizing ultrasonic energy with aspiration, are presented as a key to achieving a stable and positive clinical effect in managing chronic nasal congestion due to inferior turbinate hypertrophy, especially when complicated by nasal septum deviation. There remains considerable disagreement in the medical community regarding the merits of commonly performed traditional surgical techniques that can be more destructive. From the perspective presented, the most gentle, functionally justified technology appears to be the method of choice in the treatment of chronic nasal congestion, aiming to preserve mucosal integrity and physiological function.
Differential Diagnosis of Chronic Nasal Congestion
Chronic nasal congestion is a symptom that can arise from various underlying conditions. A thorough diagnosis is essential before considering turbinoplasty.
| Condition | Key Differentiating Features |
|---|---|
| Inferior Turbinate Hypertrophy (Compensatory, Allergic, Vasomotor) | Enlarged inferior turbinates, often boggy or firm depending on cause. May shrink with decongestants (vascular component). Often associated with septal deviation or chronic rhinitis. |
| Deviated Nasal Septum | Midline cartilage/bone is bent, causing fixed obstruction. Often leads to compensatory contralateral turbinate hypertrophy. |
| Allergic Rhinitis | Nasal itching, sneezing, watery rhinorrhea, pale/boggy turbinates. Positive allergy tests. Often responds to medical therapy. |
| Non-Allergic Rhinitis (e.g., Vasomotor, Gustatory) | Nasal congestion/rhinorrhea triggered by non-allergic stimuli. Allergy tests negative. |
| Chronic Rhinosinusitis (with or without polyps) | Persistent inflammation, purulent discharge, facial pain/pressure, hyposmia. Polyps or pus visible on endoscopy. CT shows sinus disease. |
| Adenoid Hypertrophy (especially in children/adolescents) | Nasopharyngeal obstruction, mouth breathing, snoring. Diagnosed by endoscopy or lateral neck X-ray. |
| Nasal Polyps | Pale, grape-like masses, often bilateral, causing severe obstruction and anosmia. |
| Nasal Tumors (Benign or Malignant) | Often unilateral symptoms, epistaxis, pain. Mass visible. Biopsy required. |
| Rhinitis Medicamentosa | Rebound congestion from overuse of topical decongestant sprays. History is key. |
When to Consider Turbinoplasty
Turbinoplasty, including advanced techniques like aspiration-ultrasonic intracavitary turbinoplasty, is considered when:
- Chronic nasal congestion due to documented inferior turbinate hypertrophy significantly impacts quality of life (e.g., impaired breathing, sleep disturbance).
- Conservative medical management (e.g., intranasal corticosteroids, antihistamines for allergy) has failed to provide adequate relief after a sufficient trial period (typically several weeks to months).
- Turbinate hypertrophy is contributing to or exacerbating other conditions like recurrent sinusitis or sleep-disordered breathing.
- It is performed concurrently with septoplasty to address compensatory hypertrophy and achieve optimal airway improvement.
A comprehensive evaluation by an ENT surgeon, including nasal endoscopy and potentially allergy testing or imaging, is necessary to confirm the diagnosis, rule out other causes of obstruction, and determine if turbinoplasty is the appropriate treatment.
References
- Hol MKS, Huizing EH. Treatment of inferior turbinate pathology: a review and critical evaluation of the different techniques. Rhinology. 2000 Sep;38(3):157-66.
- Passàli D, Passàli FM, Damiani V, Passàli GC, Bellussi L. Treatment of inferior turbinate hypertrophy: a randomized clinical trial. Ann Otol Rhinol Laryngol. 2003 Sep;112(9 Pt 1):683-8.
- Jackson LE, Koch RJ. Controversies in the management of inferior turbinate hypertrophy. Laryngoscope. 1999 Feb;109(2 Pt 1):218-22.
- Porto FCP, Laura P, Sall G, Ferreira G, Fonseca A, Voegels R. Submucosal turbinoplasty versus KTP laser: a comparison of two techniques for inferior turbinate hypertrophy. Braz J Otorhinolaryngol. 2009 May-Jun;75(3):426-32.
- Warwick-Brown H, Marks N. Turbinate surgery: how effective is it? A systematic review. Clin Otolaryngol. 2013 Aug;38(4):314-30.
- Spector SL. The role of turbinate surgery in the treatment of rhinitis. J Allergy Clin Immunol. 1987 Feb;79(2):305-10. (Historical context but relevant considerations)
- El-Badrawy A, El-Badrawy R, El-Shenawy A. Endoscopic ultrasound-assisted inferior turbinoplasty. J Laryngol Otol. 2005 Oct;119(10):790-4. (Context for ultrasonic techniques)
- Grymer LF, Illum P, Hilberg O. Septoplasty and compensatory inferior turbinate hypertrophy: a randomized study. Laryngoscope. 1993 Jun;103(6):609-12.
See also
- Adenoids removal surgery
- Endoscopic polyps removal
- Ethmoid sinus microsurgery
- Rhinoplasty
- Treatment of deviated nasal septum (DNS) with nasal breathing difficulty
- Turbinoplasty in deviated nasal septum (DNS) with inferior turbinates hypertrophy
- Ultrasonic septoplasty of traumatic deviated nasal septum (DNS) in the acute period