Fainting (Syncope)
Facts you should know about fainting (syncope)
- Being unconscious is not normal. If you or someone else has fainted, call 911 or go to your nearest Urgent Care.
- Symptoms of fainting include:
- Nausea
- Dizziness
- Lightheadedness
- Vision problems, for example, seeing spots or lights or blurred vision
- Fainting may be caused by a variety of medications, diseases, and conditions, but it isn't caused by a head injury, which is considered a concussion.
- Some causes of fainting can be a warning sign of a life-threatening situation. Usually, fainting is a relatively common condition, and is not life threatening.
- Most fainting spells can be easily explained, but some people never get a diagnosis or know the specific cause of the fainting spells.
What is fainting?
Fainting, "blacking out," or syncope is the temporary loss of consciousness followed by the return to full wakefulness. This loss of consciousness may be accompanied by loss of muscle tone that can result in falling or slumping over. To better understand why fainting can occur; it is helpful to explain why somebody is awake.
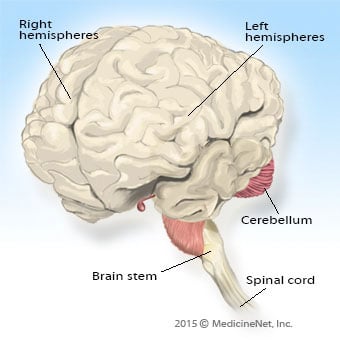
The brain has multiple parts, including two hemispheres, the cerebellum, and the brain stem. The brain requires blood flow to provide oxygen and glucose (sugar) to its cells to sustain life. For the body to be awake, an area known as the reticular activating system located in the brain stem needs to be turned on, and at least one brain hemisphere needs to be functioning. For fainting or syncope to occur, either the reticular activating system loses its blood supply, or both hemispheres of the brain are deprived of blood, oxygen, or glucose. If blood sugar levels are normal blood flow must be briefly disrupted to the whole brain or to the reticular activating system for fainting to occur.
Fainting is not caused by head trauma, since loss of consciousness after a head injury is considered a concussion. However, fainting can cause injury if the person falls and hurts themselves, or if the faint occurs while participating in an activity like driving a car.
Fainting is differentiated from seizure, during which the person may lose consciousness.

What are fainting symptoms and signs?
When a person faints they don’t know that they have passed out and fallen to the ground. Afterward, they understand what has happened.
Before the fainting episode the person may feel:
- Lightheaded
- Nausea
- Sweaty
- Weak
- Dizzy or the is room spinning (vertigo)
- Vision may fade or becomes blurred
- Hearing may be muffled
- Tingling sensations in the body
Pre-syncope or near fainting have the same symptoms, but they don't quite lose consciousness. During the fainting episode, the person may lose conscious, and there may a few twitches, which can be confused with a seizure.
The person may become confused after waking up, but it should resolve within a few seconds.
After a syncopal episode, the person should return to normal mental function. However, there may be other signs and symptoms of fainting depending on the underlying cause of fainting. For example, if the person is having a heart attack, may complain of chest pain or pressure.
What causes fainting?
Fainting causes a decrease in blood flow to the brain because
- The heart fails to pump the blood.
- The blood vessels don't have enough tone to maintain blood pressure to deliver the blood to the brain.
- There is not enough blood or fluid within the blood vessels.
- A combination of reasons one, two, or all three.

Vasovagal (vagal nerve) syncope
Vasovagal syncope is one of the most common causes of fainting. In this situation, the balance between the chemicals adrenaline and acetylcholine is disrupted. Adrenaline stimulates the body, including making the heart beat faster and blood vessels narrower, thereby increasing blood pressure. Acetylcholine does the opposite. When the vagus nerve is stimulated, excess acetylcholine is released, the heart rate slows and the blood vessels dilate, making it harder for blood to defeat gravity and be pumped to the brain. This temporary decrease in blood flow to the brain causes the fainting episode.
Pain can stimulate the vagus nerve and is a common cause of fainting (vasovagal syncope). Other noxious stimuli can do the same thing, including situational stressors. Commonly, medical and nursing students faint when observing their first operation, autopsy, or when a person or someone else is bleeding. Some people pass out when they hear bad news; others pass out when they experience the sight of blood or needles. In the Victorian age this was known as a "swoon."
Other situations commonly cause the heart rate to temporarily slow and cause a faint. Straining with urination, bowel movement, or coughing can cause a vagal response, increase acetylcholine levels and decrease blood flow to the brain.
Low blood pressure (postural hypotension), dehydration, and anemia
Fainting during pregnancy
Fainting is related to pregnancy. Likely explanations include compression of the inferior vena cava (the large vein that returns blood to the heart) by the enlarging uterus and by orthostatic hypotension.
Low blood pressure (orthostatic hypotension)
Blood vessels need to maintain their tone so that the body can withstand the effects of gravity with changes in position. When the body position changes from lying down to standing, the autonomic nervous system (the part of the brain not under conscious control), increases tone in the blood vessel walls, making them constrict, and at the same time increases the heart rate so that blood can be pumped upward to the brain. As people age, blood vessels may become less resilient, and orthostatic hypotension (relative low blood pressure with standing) may occur and cause syncope.
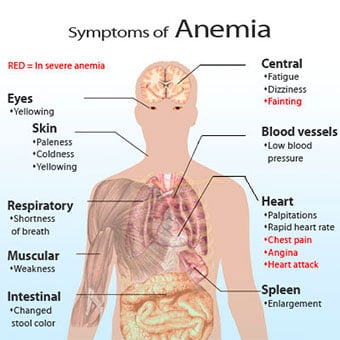
Anemia
Anemia (low red blood cell count), whether it occurs acutely from bleeding or gradually for a variety of reasons, can cause fainting because there aren't enough red blood cells to deliver oxygen to the brain.
Dehydration
Dehydration, or lack of water in the body can similarly cause fainting or syncope. This can be caused by excessive loss of water from vomiting, diarrhea, sweating, or by inadequate fluid intake. Some illnesses like diabetes can cause dehydration by excess loss of water in the urine.
Sudden cardiac arrest and heart valve and structural conditions
Sudden cardiac death
In young people, especially athletes, fainting or syncope can occur because of abnormal thickening of parts of the heart muscle (hypertrophic cardiomyopathy). This may obstruct blood when it tries to leave the heart, especially when the heart is asked to beat harder during exercise. Sudden death in athletes may be foreshadowed by episodes of syncope.
Heart valve conditions
Abnormalities with the heart valves can also cause fainting or syncope. The valves allow blood to go in the proper direction when the heart pumps. Valve diseases may include abnormal narrowing (stenosis) or leakage (insufficiency or regurgitation). Either situation can cause issues with maintaining adequate blood flow to the body.
Heart structural conditions
Structural problems with the heart can cause fainting or syncope, either because there is a problem with the ability of the heart to adequately pump blood or because of valve problems. When the heart muscle becomes damaged or inflamed it may not have the ability to pump blood to meet the body's needs. Examples include a heart attack (myocardial infarction) or cardiomyopathy, in which the heart muscle weakens.
Heart rhythm changes (rapid heartbeat and tachycardia)
- Heart rhythm changes are the most common causes of passing out, fainting, or syncope. Frequently, fainting episodes are caused by a temporary change in normal body function.
- Heart rhythm changes like tachycardia are more dangerous and potentially life-threatening causes of fainting.
- A rapid heart rate or tachycardia (tachy = fast + cardia = heart) is an abnormal heart rhythm that is generated in either the upper or lower chambers of the heart, and can be life-threatening because the heart beats too fast and may not be enough time for it to fill with blood in between heart beats, which then causes a decrease in the amount of blood that can be delivered to the body.
- Tachycardias can occur at any age and may not be related to atherosclerotic heart disease.
Vertebrobasilar artery disease
Vertebrobasilar artery disease
Blood vessels to the brain are no different than any other blood vessels in the body and are at risk for narrowing with age, smoking, high blood pressure, high cholesterol, and diabetes. While most people are aware of the carotid arteries that supply the thinking parts of the brain, another set of arteries supply the base of the brain. This vertebrobasilar system is also at risk for narrowing, and should there be a temporary disruption in the blood flow to the midbrain and the reticular activating system, fainting or syncope may occur. The vertebral arteries run to the brain in the back of the neck and are encased in bony tunnels. If blood flow in these arteries is disrupted, the brain stem and reticular activating system may turn off, causing syncope.
Electrolyte imbalance
Electrolyte and hormone abnormalities may also be responsible for syncope; however, these causes are due to their effects on the heart and blood vessels.
Other medications and drugs
Other medications or drugs may also be potential causes of fainting or syncope including those with high blood pressure that can dilate blood vessels, antidepressants that can affect heart electrical activity, and those that affect mental status like pain medications, alcohol, and cocaine.

How do medical professionals diagnose the causes of fainting?
Many conditions and events cause fainting, for example:
- Physical exam
- Diagnostic tests
- Heart monitor, for example, a Holter monitor)
- Electrocardiogram (EKG, ECG)
- CBC (complete blood count)
- Glucose levels
- Kidney function blood tests
- Thyroid blood tests
- Tilt-table test
- CT (computerized tomography)
- MRI (magnetic resonance imaging)
Heart monitors, tilt-table tests, and imaging to diagnose causes of fainting
Abnormal heart rhythm disorders (tachycardia)
Abnormal heart rhythm symptoms may go away shortly, and it is not always evident at time of the examination. Occasionally, a heart monitor (Holter monitor) can be worn as an outpatient for 24 or 48 hours or for up to 30 days (event monitor). Abnormal heart rhythms and rates may be uncovered as the potential cause of fainting.
Tilt-table test
A tilt-table test can be used to uncover orthostatic hypotension and usually is performed on an outpatient basis. The patient is placed at an angle on a table for 30-45 minutes (every institution has its own protocol) and blood pressure and pulse rate are measured with the patient in different positions.
Imaging
Depending on the suspicions that the doctor and the healthcare team have for the cause of a fainting episode, imaging of the brain may be using computerized tomography (CT scan) or magnetic resonance imaging (MRI).
Often these tests are normal so a healthcare team presumes that the cause fainting is not life-threatening. However, the doctor and patient will decide whether more testing is needed in the hospital or as an outpatient. In some people, a watchful waiting to decide whether further testing is needed.
Medical history, exams, and heart monitoring to diagnose the causes of fainting
Patient's medical history: As with most medical conditions, the history is the key in finding out why a person faints. Most fainting episodes don't happen when a person is wearing a heart monitor in front of the doctor. Often, people nearby often witness the fainting episode.
Physical exam: The doctor will look for signs or symptoms to help diagnose the cause of the fainting episode.
Causes of fainting can be diagnosed with:
- Electrocardiogram (EKG)
- Screening blood tests, for example:
- Complete blood count (CBC)
- Electrolytes
- Glucose
- Kidney function tests
- Thyroid blood tests
Heart monitoring: Heart monitoring may be done to look for heart rhythm disturbances.
- Low blood pressure (orthostatic hypotension)
- Blood pressure may be checked both lying and standing to see if the episode was caused by orthostatic hypotension.
- The heart, lung, and neurologic system may diagnose potential causes if they are abnormal.

What is the treatment for fainting?
Fainting is not normal, although the cause may not be serious. If the person is not breathing or has no pulse, call 911 or go to the nearest Urgent Care or Emergency Department. If an AED (automated external defibrillator) is available, have a bystander begin CPR.
- If the fainting episode is resolves quickly, and the person returns to normal function with no evidence of injury, it may be appropriate to contact a primary care doctor to discuss care options.
- Often, if the fainting episode does not go away quickly, the person will be placed on a heart monitor, have intravenous line (IV) fluids, and oxygen supplied. A fingerstick blood sugar may be checked to test for low blood (sugar hypoglycemia).
- Treatment for the cause of fainting will be tailored to each person.

Is it possible to prevent fainting?
Depending upon the cause, there may be opportunity to prevent fainting spells. For example:
- People who have had a vasovagal episode may be aware of the warning signs and be able to sit or lie down before passing out and prevent the fainting episode.
- Older people with orthostatic hypotension (low blood pressure when sitting or lying down) can be prevented by waiting a few seconds after changing positions, which may be all that is needed to allow the body's reflexes to react.
- If the episodes are caused by medications, they may be adjusted if they are thought to be the potential cause of fainting.
- If dehydration is the cause, drinking plenty of fluids may be enough to prevent dehydration.
- There is an increased awareness of syncope and sudden death in younger athletes due to hypertrophic cardiomyopathy. A variety of screening tests are available to assess potential risk for sudden death, but no consensus yet as to who and when to screen athletes has emerged.
