Heart Disease: Causes of a Heart Attack
What Is Heart Disease?
Heart disease refers to conditions that involve the heart, its vessels, muscles, valves, or internal electric pathways responsible for muscular contraction. Common heart disease conditions include:
- Coronary artery disease
- Heart failure
- Cardiomyopathy
- Heart valve disease
- Arrhythmias
Coronary artery disease is the main cause of heart attacks. It is the most common kind of heart disease in the U.S.
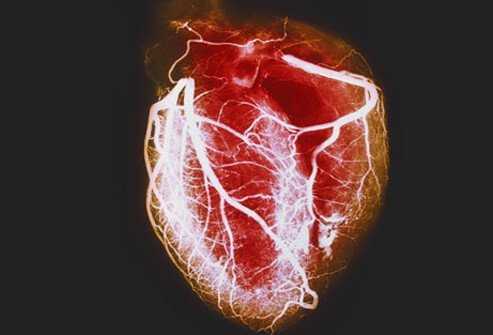
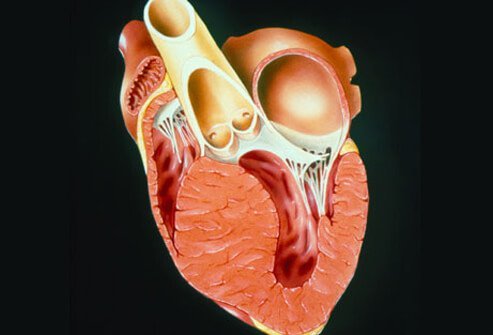
What Is a Heart Attack?

When a coronary artery becomes blocked (usually by a blood clot), an area of heart tissue loses its blood supply. This reduction of blood can quickly damage and/or kill heart tissue, so quick treatments in an emergency department and/or catheterization suite are necessary to reduce the loss of heart tissue. Loss of heart tissue due to a blockage can cause symptoms such as chest pain, shortness of breath, weakness, and even death. Quick treatments have reduced the number of deaths from heart attacks in recent years. About 790,000 people suffer from heart attacks in the U.S. each year.
Heart Attack Symptoms

The following are warning signs of a heart attack:
- Chest pain (may spread to the back, neck, arms and/or jaw)
- Dizziness
- Nausea, vomiting
- Rapid or irregular heartbeats
- Shortness of breath
- Some people may exhibit anxiety, indigestion and/or heartburn (some women may present with these as their predominant symptoms instead of chest pain)
- Weakness
- Lightheadedness
- Breaking out in a cold sweat
Women may experience different heart attack signs and symptoms than men. Jaw pain, shortness of breath, and nausea and vomiting may be more common in women who have heart attacks than men.
Heart Attack Symptoms in Women

Although some women present with symptoms of chest pain, a large number of women will not present with chest pain. Instead, women commonly have a different set of heart attack symptoms.
Know These Heart Attack Symptoms
- Arrhythmias
- Cough
- Heartburn
- Loss of appetite
- Malaise
Such symptoms in women cause delays in diagnosis if the symptoms are not considered as possible signs of heart disease. Delays in diagnosis can cause further damage to heart tissue or even death. Women should exercise, quit smoking, start exercising, and see their doctors for regular check-ups to monitor heart disease risk factors.
Coronary Artery Disease Symptoms
Coronary artery disease (CAD) occurs when plaque, a sticky substance, narrows or partially obstructs coronary arteries (like sticky material stopping up a straw) and can result in reduced blood flow. This reduced blood flow may cause chest pain (angina), a warning sign of potential heart problems such as a heart attack. Plaque may also trap small blood clots, completely blocking a coronary artery suddenly, resulting in a heart attack.
How Plaque, Blood Clots can Cause Heart Attack
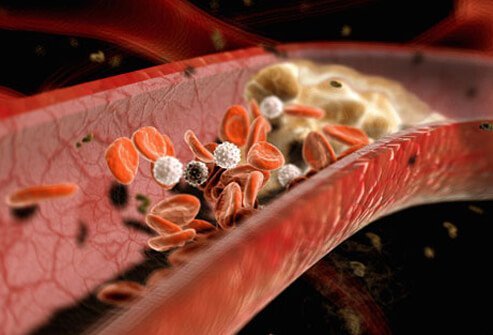
Plaque can occur in coronary and other arteries (for example, carotid arteries). Some plaque may be hard or firm on the outside, but soft and mushy or sticky on the inside. If the hard shell-like area cracks open, blood components like platelets and small blood clots form a large clot and effectively block blood flow through the artery. The heart tissue downstream from the clot then suffers from lack of blood and becomes damaged or dies.
Heart Attack Symptoms? Call 9-1-1

If you or an individual develop symptoms of a heart attack, do not delay getting medical help. Call 911 or have someone call for you. Do not drive yourself or others to a hospital as 911 emergency medical services (EMS) personnel can begin basic treatment immediately. Delaying care can result in increased heart damage or death. The sooner heart attack symptoms are identified, the sooner the patient can be treated, maximizing the chance of a good outcome.
Sudden Cardiac Arrest

A heart attack can cause other abnormalities besides blocking blood flow. For example, sudden cardiac death may occur when the heart's electrical signals become erratic (arrhythmias). When the heart tissue that is responsible for regular electrical stimulus of heart muscle contractions is damaged, the heart stops effectively pumping blood. Death usually occurs in a few minutes after the heart stops pumping blood. Consequently, rapid coronary pulmonary resuscitation (CPR) and a restoration of the organized electrical activity (usually done by electric shock with a defibrillator) may restore effective pumping of blood. This can be lifesaving for some individuals.
Erratic Heart Beat (Arrhythmia)
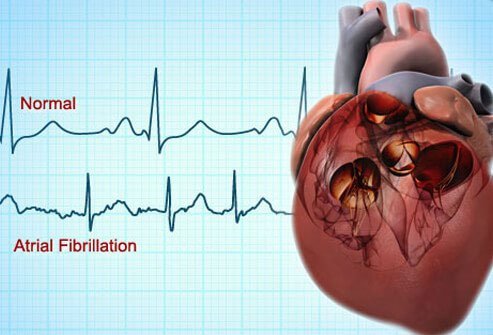
Patients who notice that their heartbeats are abnormally fast, slow, or irregular may be experiencing irregular electrical impulses termed arrhythmias. They may also have symptoms of weakness, shortness of breath, and anxiety. Arrhythmias can alter, slow or even stop the heart's ability to pump blood. Consequently, individuals with arrhythmias should seek emergency medical care especially if the arrhythmia is persistent or causes any symptoms related to heart attack symptoms such as chest pain. Ventricular fibrillation and atrial fibrillation are two examples of arrhythmias. Atrial fibrillation may increase the risk of a stroke.
Cardiomyopathy
Cardiomyopathy is a condition indicated by abnormal heart muscle. Abnormal muscles make it harder for your heart to pump blood to the rest of the body.
Main Types of Cardiomyopathy
- Dilated (stretched and thinned muscle)
- Hypertrophic (thickened heart muscle)
- Restrictive (rare problem where the heart muscle does not stretch normally so the chambers do not fill with blood properly)
Signs and Symptoms of Cardiomyopathy
- Shortness of breath
- Fatigue
- Swelling of the feet, ankles and/or legs
- Coughing when lying down
- Dizziness
- Chest pain
- Irregular heartbeats
Heart Failure
Heart failure (also termed congestive heart failure) means the pumping action of the heart cannot meet the body's demand for blood; it does not mean that the heart fails to pump - it does mean a failure in an aspect of the heart's ability to complete an otherwise normal function. The symptoms and signs are almost identical to those seen with cardiomyopathy. Most cases of heart failure are chronic, long-term heart failure.
Congenital Heart Defect

A congenital heart defect is a defect in the development of the heart as an organ that is usually first noticed at birth although some are not found until adulthood. There are many types of congenital heart defects and a few need no treatment, but others may need surgical repair. The American Heart Association lists at least 18 distinct types of congenital heart defects - many of them have additional anatomical variations.
Congenital heart defects put those patients at higher risk to develop arrhythmias, heart failure, heart valve infections, and other problems. A cardiologist (often a pediatric cardiologist) needs to be consulted on how to treat these defects. Recent advances have allowed surgeons to repair many of these defects so that the patient can go on to develop normally.
The most common congenital heart defects are problems with the heart valves and holes in the walls of the heart.
Heart Disease Testing: EKG (Electrocardiogram)
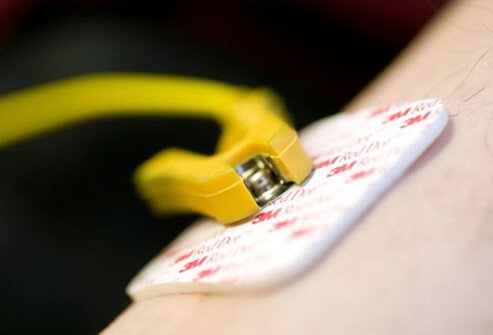
The heart's electrical activity can be seen with an EKG (also termed ECG or electrocardiogram). EKGs are tests that provide important information to the physician about the heart rhythm, damage to the heart, or a heart attack, and may provide several other important pieces of information or clues to the patient's condition. In addition, EKGs can be compared to past and future EKGs to see changes in the heart's electrical activity over time or after treatments.
Heart Disease Testing: Stress Test

A stress test measures the ability of a person's heart to respond to the body's demand for more blood during stress (exercise or work). A continual measurement of the heart's electrical activity (a continual EKG or rhythm strip) is recorded along with the heart rate and blood pressure as a person's stress (exercise) is gradually increased on a treadmill. The information helps to show how well the heart responds to the body's demands and may provide information to help diagnose and treat problems. It can also be used to see the effects of treatment on the heart.
Heart Disease Testing: Holter Monitor

Many people have intermittent symptoms such as intermittent chest pain or occasional feelings of their heart beating faster or irregularly. However, their EKG does not show any changes. To detect these intermittent changes, a device called a Holter monitor can be worn for several days to record the hearts' electrical function.
A Holter monitor is similar to a stress test, but it is worn for 1 or 2 days and provides a continual EKG-like recording of the heart's electrical activity during those days. Most doctors will ask the patient to keep a logbook of the time they do certain activities (for example, walking a mile starting at 7:20 AM and ending at 7:40 AM) and list any symptoms (for example, "experienced shortness of breath or rapid irregular heartbeats at 7:35 AM"). The Holter monitor's recordings can then be examined based on when certain symptoms occurred.
Heart Disease Testing: Chest X-ray

Chest x-rays can provide limited information about the heart's condition. Chest X-rays are used to provide the doctor with a view of both the heart and lungs to help determine if any abnormalities are present. These two X-rays show a relatively normal heart on the left. In the right X-ray, an enlarged heart (mainly the left ventricle) is easily seen and suggests the heart's main pumping chamber is not functioning normally. In addition, x-rays may show fluid accumulation in the lungs, possibly from heart failure.
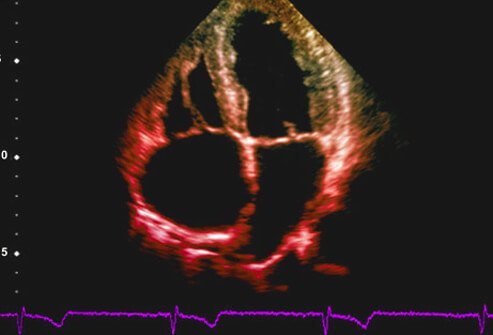
Heart Disease Testing: Echocardiogram
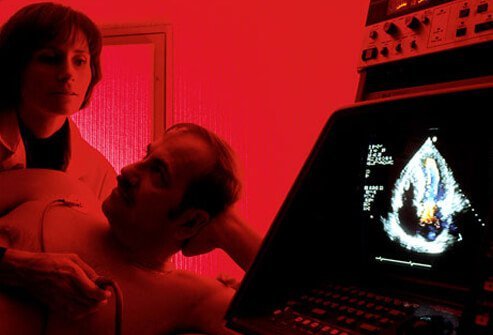
An echocardiogram is a real-time moving picture of a functioning heart made by using sound waves (ultrasound) to generate images. Echocardiograms use the same noninvasive technology used to examine the fetus during pregnancy. It can show how well heart chambers and heart valves are functioning (for example, effective or poor pumping action, blood flow through the valves), before and after treatments, as well as other features.
Heart Disease Testing: Cardiac CT Scan
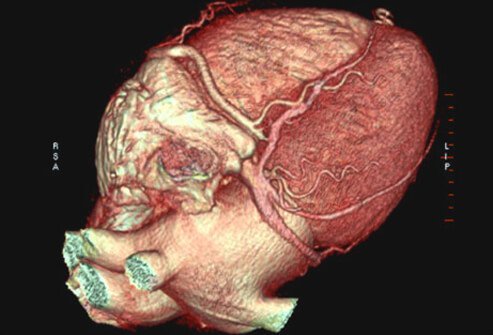
Specialized cardiac computerized tomography (CT) scans or "cardiac CTs" can provide detailed 3-D images of the heart. The images can be manipulated to look for calcium buildup (plaque) in coronary arteries or provide images of such internal structures of the heart like valves or wall thickness. CTs can also be used to examine normal heart anatomy or congenital defects. The information from a CT can provide insight into several heart disease problems.
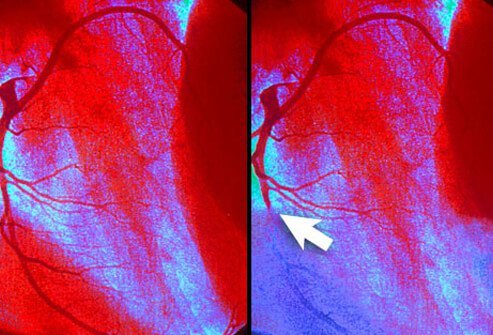
Heart Disease Testing: Cardiac Catheterization

Plaque in cardiac arteries can be a severe problem, even life-threatening, in some patients. Diagnosing plaque blockage of coronary arteries and treatment for blockages has improved the lives of many patients with coronary artery disease. Cardiac catheterization is a technique that may provide both diagnostic information and therapeutic methodology in one procedure. The technique is invasive and can be used to detect blockages in the heart that trigger heart attacks.
How Cardiac Catheterization Works
- A thin tube is placed in a blood vessel in the leg or arm and threaded into the heart and into the opening of a coronary artery.
- Dye is put into the tube and goes into the artery.
- A special X-ray machine images the dye, showing narrowing or blockage of the artery.
- The same tube may be used with special tips to open the coronary artery by angioplasty (small balloon is inflated) or used to place a wire mesh (stent) that expands to hold the artery open.
Living With Heart Disease

Most types of heart disease are chronic but slowly progressive like heart failure or cardiomyopathy. They begin with minor symptoms that often slowly worsen and require long-term medical treatment.
Symptoms That May Resist Treatment
- Ankle swelling
- Fatigue
- Fluid retention
- Shortness of breath
Lifestyle changes may become necessary (for example, home oxygen, limited activity.)
Take medications as prescribed by your doctor. Follow the doctor’s diet and exercise plan for you. If you experience new or worsening symptoms, see your doctor right away.
Heart Disease Treatment: Medicines

Advances in medicines that can help reduce the symptoms and slow the damage of heart disease have helped the majority of heart disease patients. Drugs are available to do the following:
- Lower blood pressure (anti-hypertensives)
- Lower heartbeat rates (beta blockers)
- Lower cholesterol levels to reduce plaque (diet, statins)
- Help stabilize abnormal heart rhythms (ablation, cardiac pacers)
- Reduce or prevent clotting in coronary arteries (blood thinners)
- Improve the pumping ability of a person's heart with heart disease (inotropic agents)
- Remove excess fluid from the system and decrease blood volume (diuretic)
Take cardiac medications as prescribed by your doctor to control your condition. Never skip doses of your medications or stop taking them without speaking with your doctor first.
Heart Disease Treatment: Angioplasty
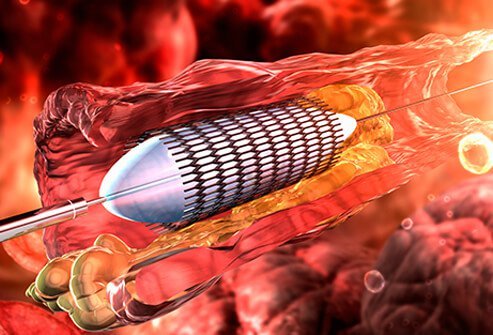
Other treatments for heart disease involve special techniques like angioplasty and stent placement.
Angioplasty Step by Step
- A thin catheter or tube (stent) is placed in a coronary artery and is threaded through an obstruction like a clot.
- A balloon is inflated and pushes aside the obstruction.
- The balloon is then deflated leaving the artery unblocked, thus allowing good blood flow.
- Often, after angioplasty, an expandable mesh tube is then inserted and expanded, reinforcing the artery to keep it from collapsing.
The nurses will apply pressure to the area where the catheter was inserted for at least 15 minutes. The patient has to lie flat on his or her back for several hours to minimize the risk of bleeding. The doctor will order the patient to avoid lifting heavy objects and avoid engaging in strenuous physical activity for a certain amount of time after the procedure, usually 1 to 2 days.
Heart Disease Treatment: Bypass Surgery

Some patient's coronary arteries are not good candidates for angioplasty and/or stents. Such patients may benefit from another treatment technique termed bypass surgery. Bypass surgery occurs when a surgeon removes a blood vessel from one part of the body (chest, legs, or arms) and uses it to connect one open part of a coronary artery to another open part, thus bypassing the area that has blocked blood flow. Often the surgeon may need to bypass more than one artery.
The decision to try and stent a coronary artery versus doing bypass surgery is usually recommended to the patient by their cardiologist and a heart surgeon. Bypass surgery is usually done if coronary arteries are narrowed or blocked in multiple places.
The procedure is known as coronary artery bypass graft (CABG). The doctor will take blood vessel from another part of the body and graft them onto the heart to bypass one, two, three, or more blocked coronary arteries. The procedure requires a stay in the hospital afterwards to recover.
Who Is at Risk for Heart Disease?

Health conditions, lifestyle, age, and family history may increase your risk for heart disease. Although men, even at a younger age, have a higher risk for heart disease than women, heart disease is still the number one killer of both sexes (about 611,000 total deaths/year). Approximately 735,000 people in the U.S. suffer a heart attack every year. People with a family history of heart disease, who smoke, and who are obese have a higher risk of developing heart disease. About half of all Americans (47%) have at least one of three key risk factor for heart disease including high blood pressure, high cholesterol, or smoking. Approximately 80 million people in the U.S. have some form of heart disease. It is the leading cause of death in men and women in the U.S.
Controllable Heart Disease Risks

Often, risk factors for heart disease can be managed or reduced through simple methods. Common risk factors for heart disease include the following:
Heart Diseases Risks You Can Control or Modify
- Diabetes
- Elevated cholesterol
- High blood pressure
- Lack of physical activity
- Stop smoking
These risk factors can be reduced simply by making healthy lifestyle choices and taking medications. Your primary care doctor can help you with your choices and medications. Stress, being overweight or obese, and alcohol consumption are contributing risk factors for heart disease. Talk to your doctor about how to decrease your risk.
Smoking Increases Heart Disease Risk

Many researchers suggest one of the best things a person can do to decrease the risk of heart disease is to stop smoking cigarettes. Smoking increases a person's risk for heart disease from 2 to about 4 times greater than nonsmokers. Smoking can damage the heart muscle, its blood vessels, can raise blood pressure, increase carbon monoxide levels, and reduce oxygen available to heart tissue.
People who do not smoke but are exposed to second-hand smoke are at greater risk for heart disease than those not exposed to second-hand smoke. Although over 135,000 people die each year from heart disease related to smoking, it is never too late to quit smoking because once you quit, your risk of heart disease begins to drop almost immediately. According to the American Heart Association, there are 480,000 deaths due to smoking-related illnesses in the U.S. every year.
Life After a Heart Attack

Don't give up activities if you have a heart attack. If a person suffers a heart attack, it is still possible to develop a healthy lifestyle. Many doctors recommend that their patients participate in a cardiac rehab program and learn how to avoid cigarettes, develop a healthy diet, and become more active. All of these changes may help a person's heart recover and function better and to reduce the chance of additional heart problems.
Approximately 20 percent of people over 45 years of age will suffer another heart attack within 5 years of suffering a first heart attack. Reduce your risk of future cardiac problems by going to follow-up appointments with your doctor and taking medications as prescribed. Participate in cardiac rehabilitation and seek support from loved ones and outside help if you need it. Manage the heart disease risk factors you can control to reduce your risk of future heart problems.
Preventing Heart Disease

Heart disease prevention and risk reduction is possible by living a healthy lifestyle. Basic components of a heart-healthy lifestyle include:
- Never smoke or stop smoking cigarettes (and using other tobacco products)
- Eat a nutritious diet (many vegetables and fruits, less fats, sugars, and meats)
- Get at least 30 minutes of exercise almost every day
- Avoid alcohol or consume no more than 1 drink per day for women and no more than 2 drinks per day for men
- If needed, achieve medical control of diabetes, high blood pressure, and cholesterol
- Encourage friends and family to help you. Maybe they could benefit from your good example!
Know your family history of heart disease. Manage your stress levels. Know the warning signs of heart attack and stroke and act fast if you notice signs and symptoms in yourself or others. Monitor your blood sugar and watch for signs and symptoms of diabetes. Be mindful of snoring; it may indicate you have sleep apnea, which increases the risk of heart disease, high blood pressure, and stroke.
Heart Disease and Diet

A major key to preventing, recovering from, and slowing heart disease is a heart-healthy diet. Most heart doctors recommend the following foods.
Heart-Healthy Foods
- Fruits
- Legumes
- Vegetables
- Whole grains
Foods That May Help Reduce Cholesterol Levels
- Nuts
- Plant oils
- Seeds
Eating fish about twice a week is a good source of protein without the fats found in red meat. Some researchers have suggested that a more vegetarian-like diet may actually reverse some aspects of coronary artery disease like plaque size. Limit your intake of saturated fat, trans fat, red meat, sugar, sugar-sweetened beverages, and sodium to protect your heart and blood vessels.
While heart disease is treatable by many methods, prevention or healing by living a reasonable lifestyle seems to be one of the best ways to reduce this widespread health problem.
Heart Disease: Causes of a Heart Attack
IMAGES PROVIDED BY:
- SPL / Photo Researchers, Inc.
- 3D Clinic
- Stephen Smith / Riser
- Nikolaevich / Photonica
- James Cavallini / Photo Researchers, Inc.
- 3D4Medical.com
- Brand X Pictures
- Medicimage
- 3D4Medical
- David Gifford / Photo Researchers, Inc.
- PDSN / Phototake -- All rights reserved.
- ERproductions Ltd
- Arno Massee / Photo Researchers, Inc.
- Corbis
- Sheila Terry / Photo Researchers, Inc.
- Living Art Enterprises, LLC and SPL / Photo Researchers, Inc.
- Doug Martin / Photo Researchers, Inc.
- Oxford Scientific
- Anthony Gray
- Jesus Tarruella / age fotostock
- Jeffrey Coolidge / Iconica
- Getty Images
- Stockbyte
- Getty Images
- Brand X Pictures
- Photosindia
- Jose Luis Pelaez/ Iconica
- Glow Wellness
- Creativ Studio Heinemann
REFERENCES:
- American Heart Association: "The American Heart Association Diet and Lifestyle Recommendations," "Cardiac Catheterization," "Cardiac Computed Tomography (Multidetector CT, or MDCT)," "Cardiac Medications," "Cardiac Procedures and Surgeries," "Chest X-Ray," "Echocardiogram (Echo)," "Exercise Stress Test," "Electrocardiogram (ECG or EKG)," "Heart Attack Symptoms in Women," "Holter Monitor," "How to Help Prevent Heart Disease at Any Age," "Life After a Heart Attack," "What Is Coronary Angioplasty?"
- Center for Disease Control: "Heart Disease," "Heart Disease Facts," "Other Conditions Related to Heart Disease."
- National Heart, Lung, and Blood Institute: "The Heart Truth," "IN BRIEF: Your Guide To Living Well With Heart Disease."
- Texas Heart Institute: "Heart Disease Risk Factors."
© 1996-2022 WebMD, LLC. All rights reserved.
Source slideshow on OnHealth
