Sjogren's Syndrome
- What Is It?
- Causes
- Risk and Complications
- Signs/Symptoms
- Diagnosis
- Treatment
- How to Prevent
- Prognosis
- Doctor and Specialists
Sjögren's syndrome facts
- Sjögren's syndrome is an autoimmune disease of salivary and tear glands.
- Sjögren's syndrome involves inflammation of glands and other tissues of the body.
- Most patients with Sjögren's syndrome are female.
- Sjögren's syndrome can be complicated by infections of the eyes, breathing passages, and mouth.
- Sjögren's syndrome is typically associated with antibodies against a variety of body tissues (autoantibodies).
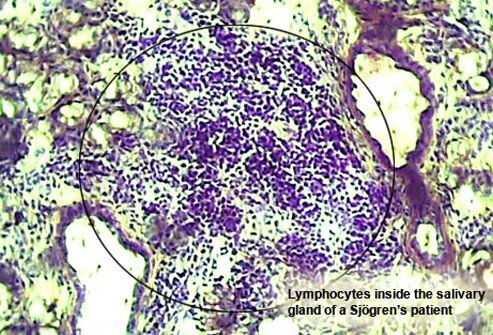
- A health care professional can diagnose Sjögren's syndrome with a saliva-gland biopsy.
- Treatment of patients with Sjögren's syndrome is directed toward relieving symptoms and complications in the particular areas of the body that are involved, such as the eyes, mouth, and vagina.
What is Sjögren's syndrome?
Sjögren's syndrome is an autoimmune disease characterized by dryness of the mouth and eyes. Autoimmune diseases feature the abnormal production of extra antibodies in the blood that are directed against various tissues of the body. The misdirected immune system in autoimmunity tends to lead to inflammation of tissues. This particular autoimmune illness features inflammation and dysfunction in glands of the body that are responsible for producing tears and saliva. Inflammation of the glands that produce tears (lacrimal glands) leads to decreased water production for tears and dry eyes. Inflammation of the glands that produce the saliva in the mouth (salivary glands, including the parotid glands) leads to decreased saliva production and dry mouth and dry lips.
Sjögren's syndrome with gland inflammation (resulting in dry eyes and mouth, etc.) that is not associated with another connective tissue disease is referred to as primary Sjögren's syndrome. Sjögren's syndrome that is also associated with a connective tissue disease, such as rheumatoid arthritis, systemic lupus erythematosus, or scleroderma, is referred to as secondary Sjögren's syndrome. Dryness of eyes and mouth, in patients with or without Sjögren's syndrome, is sometimes referred to as sicca syndrome.
What causes Sjögren's syndrome?
While the exact cause of Sjögren's syndrome is not known, there is growing scientific support for genetic (inherited) factors. The genetic background of Sjögren's syndrome patients is an active area of research. The illness is sometimes found in other family members. It is also found more commonly in families that have members with other autoimmune illnesses, such as systemic lupus erythematosus, autoimmune thyroid disease, type I diabetes, etc. Most patients with Sjögren's syndrome are female.
What are risk factors for developing Sjögren's syndrome?
The main risk factor for the development of Sjögren's syndrome is being a member of a family that is already characterized as having autoimmune illnesses. This does not mean that it is predictable that a member of a family with known autoimmunity will develop the disease, only that is more likely than if there were no family members with known autoimmunity. Accordingly, it is likely that certain genes that are inherited from ancestors can predispose one to the development of Sjögren's syndrome. It should also be noted that Sjögren's syndrome can also be sporadic and occur in a person from a family with no known autoimmunity.
What are Sjögren's syndrome symptoms and signs?
Symptoms of Sjögren's syndrome can involve the glands, as above, but there are also possible effects of the illness involving other organs of the body (extraglandular manifestations).
When the tear gland (lacrimal gland) is inflamed from Sjögren's, the resulting eye dryness can progressively lead to symptoms such as eye irritation, decreased tear production, a "gritty" sensation, eye infection, and serious abrasion of the dome of the eye (cornea). Dry eyes can lead to infections of the eyes and inflammation of the eyelids (blepharitis). The condition of having dry eyes is medically referred to as xerophthalmia. When the eyes become inflamed from dryness, it is referred to as keratoconjunctivitis sicca.
Inflammation of the salivary glands can lead to the following symptoms and signs:
- mouth dryness,
- swallowing difficulties,
- dental decay,
- cavities,
- gum disease,
