Raynaud's Phenomenon
- Definition
- Raynaud's Phenomenon vs. Disease
- Causes
- Risk Factors
- Symptoms & Signs
- Tests
- Specialists
- Treatment
- Prognosis
- Prevention
- Research
Facts you should know about Raynaud's phenomenon
- Raynaud's phenomenon is a type of vascular disease characterized by a pale to blue to red sequence of color changes of the digits, most commonly after exposure to cold.
- Raynaud's phenomenon occurs because of spasm of blood vessels.
- The cause of Raynaud's phenomenon is unknown, although abnormal nerve control of blood-vessel diameter and nerve sensitivity to cold are suspected of being involved.
- Symptoms of Raynaud's phenomenon depend on the severity, frequency, and duration of the blood-vessel spasm.
- There is no blood test for diagnosing Raynaud's phenomenon.
- Treatment of Raynaud's phenomenon involves protection of the digits, medications, and avoiding emotional stresses, smoking, cold temperature, and tools that vibrate the hands.
What is Raynaud's phenomenon vs. Raynaud's disease?
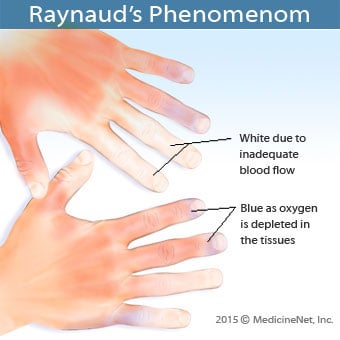
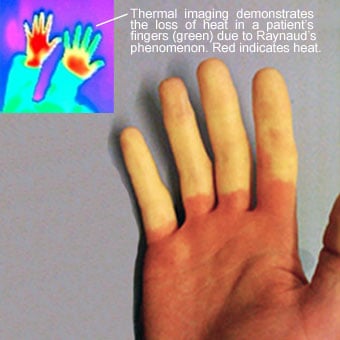
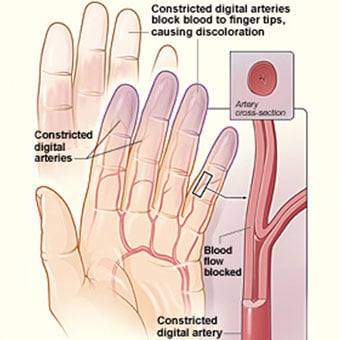
Raynaud's phenomenon (RP) is a disorder resulting in vasospasm, a particular series of discolorations of the fingers and/or the toes after exposure to changes in temperature (cold or hot) or emotional events. Most people with RP have a sensitivity to cold. Skin discoloration occurs because an abnormal spasm of the blood vessels causes diminished blood flow to the local tissues. Initially, the digit(s) involved turning white because of the diminished blood flow. The digit(s) then turn blue (cyanosis) because of a prolonged lack of oxygen. Finally, the blood vessels reopen, causing a local "flushing" phenomenon, which turns the digit(s) red. This three-phase color sequence (white to blue to red), most often upon exposure to cold temperature, is characteristic of RP.
Raynaud's phenomenon most frequently affects women, especially in the second, third, or fourth decades of life. People can have Raynaud's phenomenon alone or as a part of other rheumatic diseases. Raynaud's phenomenon in children is essentially identical to Raynaud's phenomenon in adults. When it occurs alone, it is referred to as "Raynaud's disease" or primary Raynaud's phenomenon. When it accompanies other diseases, it is called secondary Raynaud's phenomenon.
What causes Raynaud's phenomenon?
The causes of primary Raynaud's phenomenon and secondary Raynaud's phenomenon are unknown. Both abnormal nerve control of the blood-vessel diameter and nerve sensitivity to cold exposure have been suspected as being contributing factors. The characteristic color changes of the digits are in part related to initial blood-vessel narrowing due to spasm of the tiny muscles in the wall of the vessels, followed by sudden opening (dilation), as described above. The small arteries of the digits can have microscopic thickness of their inner lining, which also leads to abnormal narrowing of the blood vessels.
What are risk factors from Raynaud's phenomenon?
Risk factors for Raynaud's phenomenon include injury from frostbite and vibrating tools, medications (bleomycin [Blenoxane]), propranolol (Inderal), ergotamine), and having rheumatic autoimmune diseases such as scleroderma, systemic lupus erythematosus, Sjögren's syndrome, mixed connective tissue disease, and rheumatoid arthritis.
What conditions have been associated with Raynaud's phenomenon?
Raynaud's phenomenon has been seen with a number of conditions, including rheumatic autoimmune diseases (scleroderma, rheumatoid arthritis, lupus, and mixed connective tissue disease), hormone imbalance (hypothyroidism and carcinoid), trauma (frostbite, vibrating tools), medications (propranolol [Inderal], estrogens without additional progesterone, bleomycin [Blenoxane] used in cancer treatment, and ergotamine used for headaches), nicotine, and even rarely with cancers.

What are Raynaud's phenomenon symptoms and signs?
Symptoms of RP depend on the severity, frequency, and duration of the blood vessel spasm. Most patients with mild disease only notice skin discoloration upon cold exposure when digits turn white, then blue, and then flush red when the blood vessels reopen. They may also experience mild tingling and numbness of the involved digit(s) that will disappear once the color returns to normal. When the blood-vessel spasms become more sustained, the sensory nerves become irritated by the lack of oxygen and can cause pain in the involved digit(s). Rarely, poor oxygen supply to the tissue can cause the tips of the digits to ulcerate. Ulcerated digits can become infected. With continued lack of oxygen, gangrene of the digits can occur.
Less common areas of the body that can be affected by RP include the nose, ears, and tongue. While these areas rarely develop ulcers, they can be associated with a sensation of numbness and pain.
Patients with secondary RP can also have symptoms related to their underlying diseases. RP is the initial symptom of a majority of patients with scleroderma, a skin and joint disease. Other rheumatic diseases frequently associated with RP include lupus, rheumatoid arthritis, and Sjögren's syndrome.
What tests do health care professionals use to diagnose Raynaud's phenomenon?
In patients with the characteristic sequence of skin-color changes of the digits upon cold exposure, diagnosing RP is not difficult. Sometimes, certain patterns in the tiny blood vessels (capillaries) adjacent to the fingernails of patients with RP can be seen using a magnifying viewing instrument. Abnormal nail-fold capillary patterns can suggest the possibility of an associated rheumatic condition. There is, however, no single blood test to help the doctor to confirm the diagnosis. The doctor can order certain blood tests (for example, sedimentation rate, rheumatoid factor, antinuclear antibody, thyroid hormone levels, and protein levels) to exclude associated rheumatic diseases and thyroid disorders. The doctor can also perform certain maneuvers with the patient's extremities to exclude pinched blood vessels that can produce symptoms that mimic RP, such as in thoracic outlet syndrome.
Typically, patients with Raynaud's phenomenon that is a manifestation of a rheumatic disease have elevated blood sedimentation rates and antinuclear antibodies. Furthermore, capillary nail-fold abnormalities can frequently be found as described above.
What specialties of doctors treat Raynaud's phenomenon?
Doctors who treat Raynaud's phenomenon include general-medicine physicians, family medicine physicians, internists, rheumatologists, and hand surgeons.

What is the treatment for Raynaud's phenomenon?
Management of Raynaud's phenomenon involves preventing the spasm of the blood vessels by protecting the fingers and the toes from cold, trauma, and infection. Medications that can aggravate blood vessel spasm should be avoided by patients with RP. In patients with persistent symptoms, medications that dilate the blood vessels (angiotensin-receptor blockers and calcium channel blockers [amlodipine, nifedipine, felodipine]) can be administered.
Patients with Raynaud's phenomenon who have no symptoms other than the color changes of extremities may require only home-remedy measures to prevent complications. Prevention measures are important in primary and secondary RP regardless of the severity. Simple initial care involves keeping the body warm, especially the extremities. Warm clothing in colder environments is essential. Cotton gloves can be helpful while searching the freezer. Headwear can help the body retain heat by minimizing heat dissipation. Room temperatures should not be too cool. Rubber gloves protect the hands and prevent cooling while washing dishes. Barefoot walking should be minimized. Compression of the blood vessels by tight-fitting wrist bands, rings, or footwear should be avoided.
Note: Some energy companies offer some discounts on utility bills for those who suffer from Raynaud's phenomenon because of the additional heating requirements.
Those with RP should guard their hands and feet from direct trauma and wounds. Any wounds or infections should be treated early to prevent more serious infections. Avoiding emotional stresses and tools that vibrate the hand may reduce the frequency of attacks. Biofeedback can also help to decrease the severity and frequency of RP in some patients.
Direct and indirect (passive or secondhand smoke) smoking should be avoided by patients with RP. The chemicals in tobacco smoke can cause blood-vessel constriction and lead to atherosclerosis (hardening of the arteries), which can further impair oxygen supply to the extremities.
Care of the nails must be done carefully to avoid injuring sensitive toes and fingertips. Ulcers on the tips of the digits should be monitored closely by the doctor. These can become infected. Gently applied finger splints are used to protect ulcerated areas. Ointments that open the blood vessels (nitroglycerin ointment) are sometimes used on the sides of severely affected digits to allow increased blood supply and healing.
Patients with persistent or bothersome symptoms may be helped by taking oral medications that open (dilate) blood vessels. (Sometimes these medications are decreased or eliminated when the environment is warmer, such as during summer months.) These include calcium antagonists (or calcium channel blockers), such as diltiazem (Cardizem, Dilacor), nicardipine (Cardene), nifedipine (Procardia), and other medicines used in blood pressure treatment, such as methyldopa (Aldomet) and prazosin (Minipress). Recent research has shown that the blood-pressure drug losartan (Cozaar, Hyzaar) can reduce the severity of episodes of RP.
Medications that thin the blood, such as low doses of aspirin or dipyridamole (Persantine), are sometimes helpful.
Some patients with persistent symptoms can benefit by adding a medication called pentoxifylline (Trental), which makes the red blood cells more pliable and thereby improving circulation.
Severe RP can lead to gangrene and the loss of digits from lack of blood supply. With severe disease, nerve surgery called "sympathectomy" is sometimes considered. In this procedure, to prevent blood-vessel spasm, the nerves that stimulate the constriction of the vessels (sympathetic nerves) are surgically interrupted. Usually, this is performed during an operation that is localized to the sides of the base of the fingers at the hand. Through small incisions, the tiny nerves around the blood vessels are stripped away. This procedure is referred to as a digital sympathectomy.
What is the prognosis (outlook) for Raynaud's phenomenon?
The outlook for those affected by Raynaud's phenomenon depends on its severity and whether or not there is associated underlying medical illness. Most people affected by Raynaud's phenomenon do very well in response to simple measures, with or without medications.
Is it possible to prevent Raynaud's phenomenon?
Raynaud's phenomenon can be prevented by avoiding the precipitating factors, such as cold or heat exposure, smoking, etc.
Certain medications should be avoided. Medications that can aggravate symptoms of RP by leading to increased blood-vessel spasm include over-the-counter cold and weight-control preparations, such as pseudoephedrine (Actifed, Chlor-Trimeton, CoTylenol, and Sudafed). Beta blockers, medicines used for high blood pressure and heart disease, can also worsen RP. These include atenolol (Tenormin), metoprolol (Lopressor), nadolol (Corgard), and propranolol.
What research is being done on Raynaud's phenomenon?
Researchers have reported finding a substantial genetic (inherited) contribution both to the symptoms of RP and to the associated blood-vessel changes of patients with Raynaud's phenomenon.
Other researchers are studying nitric oxide and its potential relationship to Raynaud's phenomenon. A gel is being studied which might promote local production of nitric oxide in involved digits. The local nitric oxide, it seems, may open the blood vessels and improve the impaired circulation.
For further information about Raynaud's phenomenon, please visit the following site:
The Arthritis Foundation (http://www.arthritis.org)
Or you can write to:
The Arthritis Foundation
PO Box 19000
Atlanta, Georgia 30326