Does Rheumatoid Arthritis Cause IBD?
Rheumatoid arthritis (RA) is an autoimmune inflammatory joint condition that causes pain, swelling, tenderness, and redness of multiple joints in the body. An autoimmune condition occurs when the body suffers from dysregulation of the immune system and attacks its own proteins. Both RA and inflammatory bowel disease (IBD) are autoimmune conditions. According to multiple studies, many immune-mediated diseases have overlapping pathologies. Hence, some people affected with RA may develop other autoimmune conditions, such as IBD. However, people are more likely to have other issues with their digestive system that may not necessarily be caused by IBD.
How can rheumatoid arthritis affect your digestive tract?
Role of inflammation
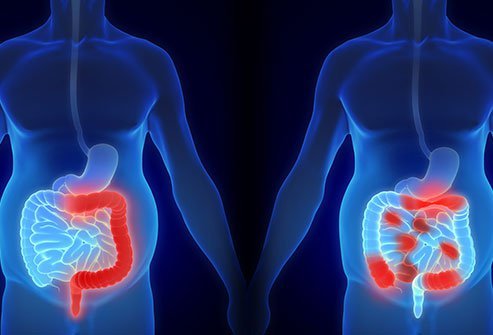
Studies show that inflammatory bowel disease (IBD) and rheumatoid arthritis (RA) can coexist in some people. IBD represents two conditions: Crohn’s disease and ulcerative colitis. These are characterized by chronic inflammation of the digestive tract. It is the “chronic” inflammation that is common to both conditions. The same inflammation that targets your joints in RA may also affect your digestive system and lead to IBD.
Rheumatoid vasculitis is a condition that causes inflammation of the blood vessels. It can also affect the gastrointestinal (GI) tract and result in symptoms, such as abdominal pain, nausea, vomiting and diarrhea, and weight loss. Controlling RA by targeting the inflammation alleviates these symptoms as well.
Role of genes and environment
Common genetic (genes, such as HLA-DRB1 and TYK2) and environmental factors may play a role in the development of both RA and IBD.
Can rheumatoid arthritis medications affect your digestive system?
It is common to experience gastrointestinal symptoms as side effects of medications for rheumatoid arthritis (RA). The common medications include:
- Nonsteroidal anti-inflammatory drugs (NSAIDs): Frequent and prolonged use of NSAIDs can cause gastritis and peptic ulcer disease.
- Steroids: High doses of steroids for prolonged periods may result in gastric ulcer, gastrointestinal (GI) perforation (GI bleeding), and pancreatitis. The risk increases if you are also taking NSAIDs.
- Disease-modifying antirheumatic drugs (DMARDs): Methotrexate can cause diarrhea, nausea, vomiting, and abdominal pain.
- Immunotherapy (biologics): Many drugs used for immunotherapy to treat RA can produce side effects, such as nausea, diarrhea, or abdominal cramps. Serious complications include GI perforations and bowel obstruction.
You should discuss all the possible risks and benefits of taking any of these medications with your doctor as part of your shared decision-making process.
How can you alleviate gastrointestinal problems in rheumatoid arthritis?
If you want to alleviate your gastrointestinal (GI) symptoms, it is important to follow your doctor’s instructions for keeping your arthritis under control. Also, let your doctor know if you experience any new GI symptoms after starting the medications. They may change your medication or put you on drugs, such as proton-pump inhibitors, that work to reduce your nausea. They may also recommend certain dietary modifications to minimize your GI complaints.
