Diverticulitis (Diverticulosis, Diverticular Disease)
Facts you should know about diverticulosis and diverticulitis
- Most people with diverticulosis (diverticular disease) have few or no symptoms, and the symptoms that occur with diverticulosis probably are not caused by the diverticula, even though this has been referred to as "diverticular disease." The symptoms of diverticulitis include:
- When diverticulosis is associated with inflammation and infection it is called "diverticulitis."
- Diverticulitis as well as diverticular disease can be diagnosed with barium X-rays, sigmoidoscopy, colonoscopy, or CT scan.
- Treatment of diverticulitis and diverticular disease can include high fiber diet, and anti-spasmodic drugs.
- Foods to eat in your diet that are thought to prevent diverticulitis flares include fruits and vegetables, legumes, and whole grains.
- It has been suggested that people with diverticulitis should avoid eating seeds, nuts, and corn; however, there is little evidence to support this recommendation.
- When diverticulosis is associated with inflammation and infection the condition is called diverticulitis.
- Complications of diverticulosis and diverticulitis include rectal bleeding, abdominal infections, and colon obstruction.
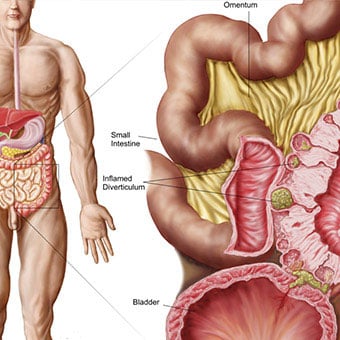
What is diverticulosis? What does it look like (pictures)?
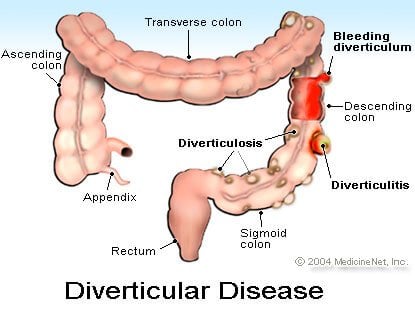
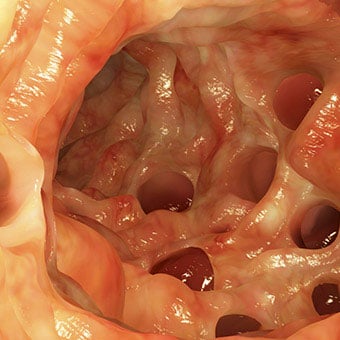
The colon (large intestine or large bowel) is a long tube-like structure approximately 6 feet in length that stores and then eliminates waste material left over after digestion of food in the small intestine takes place. It is thought that pressure within the colon causes bulging pockets of tissue (sacs) that push out from the colonic walls as a person ages. A small bulging sac pushing outward from the colon wall is called a diverticulum. More than one bulging sac is referred to in the plural as diverticula. Diverticula can occur throughout the colon but are most common near the end of the left colon, referred to as the sigmoid colon, in Western countries. In Asia, the diverticula occur mostly on the right side of the colon. The condition of having these diverticula in the colon is called diverticulosis.
Diverticula are common in the Western world but are rare in areas such as Asia and Africa. Diverticula increase with age. They are uncommon before the age of 40, but are seen in more than 74% of people over the age of 80 years in the U.S. A person with diverticulosis usually has few or no symptoms. The most common symptoms associated with diverticulosis are abdominal pain, constipation, and diarrhea. In most people with diverticular disease, the symptoms may be due to the concomitant presence of irritable bowel syndrome (IBS) or abnormalities in the function of the muscles of the sigmoid colon; simple diverticula should cause no symptoms. Occasionally, bleeding originates from a diverticulum, and it is referred to as diverticular bleeding.
What is diverticulitis?
When a diverticulum ruptures and inflammation and infection sets in around the diverticulum, the condition is called diverticulitis. Often, a person with diverticulitis has symptoms and signs that include:
- Abdominal pain
- Abdominal tenderness
- An obstruction in the colon (colonic obstruction)
- An elevated white blood cell count in the blood, and fever.
What causes diverticula and how do diverticula form?
The muscular wall of the colon grows thicker with age, although the cause of this thickening is unclear. It may reflect the increasing pressures required by the colon to eliminate feces. For example, a diet low in fiber can lead to small, hard stools which are difficult to pass and which require increased pressure to pass. The lack of fiber and small stools also may allow segments of the colon to close off from the rest of the colon when the colonic muscle in the segment contracts. The pressure in these closed-off segments may become high since the increased pressure cannot dissipate to the rest of the colon. Over time, high pressures in the colon push the inner intestinal lining outward (herniation) through weak areas in the muscular walls. These pouches or sacs that develop are called diverticula.
Lack of fiber in the diet has been thought to be the most likely cause of diverticula, and there is a good correlation among societies around the world between the amount of fiber in the diet and the prevalence of diverticula. Nevertheless, studies have not found similar correlations between fiber and diverticula within individual societies. Many people with diverticular disease have excessive thickening of the muscular wall of the colon where the diverticula form. The muscle also contracts more strongly. These abnormalities of the muscle may be contributing factors in the formation of diverticula. Microscopic examination of the edges of the diverticula show signs of inflammation, and it has been suggested that inflammation may be important for the formation of the diverticula and not just the result of them.

What are diverticulitis symptoms?
Most patients with diverticulosis have few or no symptoms. The diverticulosis in these individuals is found incidentally during tests for other intestinal problems. It has been thought as many as 20% of individuals with diverticulosis will develop symptoms related to the diverticulosis, primarily diverticulitis; however, the most recent study suggests that the incidence is closer to 5%.
The most common signs and symptoms of diverticulitis include:
- Abdominal pain (left lower abdomen)
- Abdominal tenderness (left lower abdomen)
- Fever
- Elevated white blood cell count in the blood
- Constipation or, sometimes, diarrhea.

Is there a diverticulitis diet? What food should be avoided to prevent diverticulitis? What foods prevent flares?
Once formed, diverticula do not go away; they are permanent. No treatment has been shown to treat or prevent diverticular disease or diverticulitis. Nevertheless, recommendations have been made in regard to which foods to eat, and which foods to avoid.
Foods to eat that may prevent flares
Since one theory holds that it is reduced fiber in the diet that causes diverticulitis, diets high in fiber are the most recommended treatment for diverticula. Fiber clearly increases stool bulk and prevents constipation, and, if it really reduces pressures in the colon, theoretically it may help prevent further diverticula formation or worsening of the diverticular condition. Foods high in fiber include:
- Fruits and vegetables
- Legumes/beans, (for example, lima, kidney, cannellini, and red kidney beans; chickpeas, split peas, and tofu)
- Whole grains (for example, brown rice, cracked wheat, oatmeal, quinoa, rolled oats, rye bread, wild rice; and whole wheat bread, cereal, crackers, pasta, and tortillas)
Foods to avoid with diverticulitis
Some doctors recommend avoiding nuts, corn, and seeds, which are thought by some to plug diverticular openings and cause diverticulitis, but there is little evidence to support this recommendation. Nevertheless, foods frequently recommended to be avoided include:
- Popcorn
- Poppy seeds
- Sesame seeds
What about probiotics and diverticulitis or diverticular disease?
Because inflammation has been found at the edges of diverticula, it has been speculated that colonic bacteria may be playing a role in the rupture of diverticula by promoting inflammation. This has led some people to further speculate that changing the bacteria in the colon might reduce inflammation and rupture and to suggest treatment with probiotics and/or prebiotics; however, there is not enough evidence of a benefit of probiotics yet to recommend treatment with probiotics of patients with diverticular disease.
What are the more serious complications of diverticulitis?
More serious complications of diverticulitis include:
- Collection of pus (abscess) in the pelvis where the diverticulum has ruptured
- Colonic obstruction due to extensive inflammation
- Generalized infection of the abdominal cavity (bacterial peritonitis)
- Bleeding into the colon
A diverticulum can rupture, and the bacteria within the colon can spread into the tissues surrounding the colon. This is then called diverticulitis. Constipation or diarrhea also may occur with the inflammation. A collection of pus can develop around the ruptured diverticulum, leading to formation of an abscess, usually in the pelvis. Inflammation surrounding the colon also can lead to colonic obstruction. Infrequently, a diverticulum ruptures freely into the abdominal cavity causing a life threatening infection called bacterial peritonitis. On rare occasions, the inflamed diverticulum can erode into the urinary bladder, causing bladder infection and passing of intestinal gas in the urine. Even more rarely the diverticulum can rupture into the vagina.
Diverticular bleeding occurs when the expanding diverticulum erodes into a blood vessel within the wall of the diverticulum. Rectal passage of red, dark or maroon-colored blood and clots occur without any associated abdominal pain if there is no diverticulitis, but bleeding into the colon also may occur during an episode of diverticulitis. Blood from a diverticulum of the right colon may cause the stool to become black in color. Bleeding may be continuous or intermittent, lasting several days.
Patients with active bleeding usually are hospitalized for observation. Intravenous fluids are given to support the blood pressure. Blood transfusions are necessary for those with moderate to severe blood loss. In a rare individual with brisk and severe bleeding, the blood pressure may drop, causing dizziness, shock, and loss of consciousness. In most patients, bleeding stops spontaneously and they are sent home after several days in the hospital. Patients with persistent, severe bleeding require surgical removal of the bleeding diverticulum although several nonsurgical treatments have been suggested.

What tests and imaging procedures diagnose diverticulitis and diverticulosis?
The signs and symptoms of diverticulitis are common and distinctive enough that the presence of diverticulitis is usually suspected. If suspected, the diagnosis can be confirmed by a variety of tests. Barium X-rays (barium enemas) can be performed to visualize the colon. Diverticula are seen as barium filled pouches protruding from the colon wall.
Direct visualization of the inside of the colon and the openings of the diverticula can be done with flexible tubes inserted through the rectum and advanced into the colon. Either short tubes (sigmoidoscopes) or longer tubes (colonoscopes) may be used to assist in the diagnosis and to exclude other diseases that can mimic diverticular disease.
In patients suspected of having diverticulitis ultrasound, CT (computerized tomograph) and MRI (magnetic resonance imaging) scans of the abdomen and pelvis can be ordered to detect inflammation of the tissues surrounding the ruptured diverticulum or collections of pus.
What home treatment or remedies help soothe diverticulitis symptoms?
Patients may have multiple episodes of diverticular disease or diverticulitis, and may be difficult to distinguish between the two. Milder episodes of pain may be treated at home with bed rest, medications for pain and spasm, and a clear liquid diet. Patients should take their temperature frequently and push on their lower left abdomen where most diverticula are located. At the first sign of fever or increasing tenderness--signs of inflammation--a doctor should be consulted immediately for a possible visit to his office and/or the initiation of antibiotics; there is nothing as valuable as a physical examination by the doctor to help make decisions about further treatment or hospitalization.
What medications treat diverticulitis and diverticulosis?
Most patients with diverticulosis have minimal or no symptoms, and do not require any specific treatment. A normal fiber diet is advisable to prevent constipation and perhaps prevent the formation of more diverticula.
Patients with mild symptoms of abdominal pain due to muscular spasm in the area of the diverticula may benefit from anti-spasmodic drugs, for example,
- chlordiazepoxide (Librax),
- dicyclomine (Bentyl),
- atropine, scopolamine, phenobarbital (Donnatal), and
- hyoscyamine (Levsin).
Learn more about: phenobarbital
Learn more about: phenobarbital
When diverticulitis occurs, antibiotics usually are needed. Oral antibiotics are sufficient when symptoms are mild. Some examples of commonly prescribed antibiotics include
- ciprofloxacin (Cipro),
- metronidazole (Flagyl),
- cephalexin (Keflex), and
- doxycycline (Vibramycin).
Learn more about: Cipro | Flagyl | Keflex | Vibramycin
What are other treatments for diverticulitis?
Liquid or low fiber foods are advised during acute attacks of diverticulitis. This is done to reduce the amount of material that passes through the colon, which at least theoretically, may aggravate the diverticulitis. In severe diverticulitis with high fever and pain, patients are hospitalized and given intravenous antibiotics. Surgery is needed for patients with persistent bowel obstruction, bleeding, or abscess not responding to antibiotics.

What is the surgical treatment for diverticulitis?
Diverticulitis that does not respond to medical treatment requires surgical intervention. Surgery usually involves drainage of any collections of pus and resection (surgical removal) of the segment of the colon containing the diverticula, usually the sigmoid colon. Surgical removal of the bleeding diverticulum also is necessary for those with persistent bleeding. In patients needing surgery to stop persistent bleeding, it is important to determine exactly where the bleeding is coming from in order to guide the surgeon.
Sometimes, diverticula can erode into the adjacent urinary bladder, causing severe recurrent urine infection and passage of gas during urination. This situation also requires surgery.
Sometimes, surgery may be suggested for patients with frequent, recurrent attacks of diverticulitis leading to multiple courses of antibiotics, hospitalizations, and days lost from work. During surgery, the goal is to remove all, or almost all, of the colon containing diverticula in order to prevent future episodes of diverticulitis. There are few long-term consequences of resection of the sigmoid colon for diverticulitis, and the surgery often can be done laparoscopically, which limits post-operative pain and time for recovery.



