What Are the Side Effects of ParaGard?
The most typical side effects of ParaGard, an intrauterine device (IUD), are heavier, crampy and longer periods. Most adverse effects normally go away after a few months. However, if a woman has significant menstrual bleeding or misses her periods, she should see a doctor because it could be due to pregnancy or a missed abortion.
Thousands of American women use the copper IUD ParaGard to provide long-term birth control and pregnancy prevention. Here are some of the most common side effects of the device:
- Spotting between periods
- Pelvic inflammatory disease (PID) is characterized by abdominal pain, foul-smelling discharge and infertility
- Vaginal discharge
- Infections (bacterial vaginosis)
- Pain during sex
- Allergic reactions (rash, discharge per vaginum and joint pain)
- Anemia
- Weakness
- Light-headedness
- Menstrual cramps
- Back pain
- Perforation of the uterus
- The device or a portion of the device migrates, causing organ perforation (such as the colon) and organ damage
- Leftover copper wire in the body may cause inflammation and injury
- Scarring
- Difficulty removing the device, which may require in some cases
- Ectopic pregnancy (a pregnancy when a fertilized egg implants and grows outside the main cavity of the uterus)
- Miscarriage
- Loss of reproductive health (infertility)
- Death is reported in some cases
Studies published in the American Journal of Obstetrics and Gynecology concluded that ParaGard has the potential for serious injuries and complications. The device's reaction within the body, complications during removal or the device itself might cause problems.
ParaGard users may have a higher rate of expulsion of the IUD and unintended pregnancies than those who use other types of IUDs. ParaGard does not protect from sexually transmitted illnesses. If a woman uses or is considering using ParaGard, they should be aware of the hazards.
How effective is ParaGard IUD insertion?
According to studies, ParaGard is 99 percent efficient in preventing pregnancy (as long as it stays in place). It is thought to be more effective than birth control tablets and emergency contraception. It's one of five intrauterine devices (IUDs) on the market in the United States, and it's the only one that's fully hormone-free.
ParaGard can last up to 10 years, however, if it breaks, passes through the uterus or perforates, it loses its contraceptive function. Once the device is removed entirely and safely, the woman may be able to become pregnant from unprotected sex immediately (unless there are unrelated issues, such as age or underlying conditions that reduce fertility).
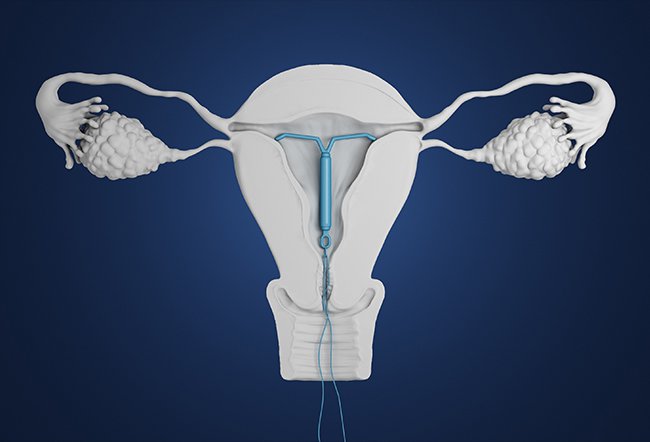
ParaGard is a little T-shaped device made of monofilament threads that do not prevent ovulation. Instead, its copper wires keep sperm from reaching an egg through the fallopian tubes. In addition, it can assist to prevent the implantation of the egg inside the uterus.
How painful is a ParaGard IUD insertion?
The T-shaped device is normally inserted into a woman's uterus (womb) by a gynecologist, during which the entire procedure is usually rapid. However, the woman may experience some amount of discomfort.
When the womb's opening (cervix) is stretched, it is painful for a while. For most women, this lasts for a few seconds and can feel like a searing ache. The discomfort level during intrauterine device (IUD) insertion is 2/10 to 4/10 on the pain scale.
An IUD is a straightforward treatment that takes only a few minutes to complete.
- A doctor or nurse may inspect the vaginal area before they place the IUD.
- The procedure of inserting an IUD can be painful; thus, the doctor or nurse may give the woman a local anesthetic to alleviate the discomfort.
- The doctor or nurse implants the coil through the cervix after they put a speculum into the vaginal canal (neck of the womb).
- It can make the woman feel a little uneasy and induce period-like aches thereafter. However, pain relievers can help with cramping.
- After getting an IUD, the woman may bleed for a few days.
How painful is the ParaGard IUD removal process?
Removing an intrauterine device (IUD) is a simple procedure with no pain; however, it should only be performed by a qualified medical professional. It is usually less unpleasant to remove an IUD than it is to put one in.
- The woman may be requested to lie down on a table with her knees bent and legs apart.
- The doctor or nurse may insert a speculum into the vaginal opening to enlarge it.
- Threads from the IUD may protrude into the vaginal canal from the cervix (womb's neck).
- The doctor may gently tug on the strings and pull out the gadget using a specific gripping instrument.
- The arms of an IUD fold up when it goes out, making it T-shaped.
- If the doctor can't see or reach the threads, they may pull the threads with a special hook or other equipment.
- In rare situations, the IUD may become lodged in the uterine wall and be difficult to remove. Doctors frequently administer an anesthetic to the woman and use forceps to expand her cervix and pull it out. To remove the IUD, the doctor may use a thin, illuminated scope to check within the vagina and uterus.
- For a few days or weeks after the IUD is removed, the woman may experience moderate cramps, spotting or light bleeding, and the doctor may advise an over-the-counter pain treatment.
